Rethinking IV Fluid Resuscitation in Sepsis
SUMMARY
- Fluid resuscitation is a key component in the management of sepsis and shock to improve fluid volume.
- The risks of fluid overload may contribute to poorer outcomes.
- Despite widespread support for fluid resuscitation, data supporting large volumes is limited.
REVIEW
- The Surviving Sepsis Campaign recommends patients receive 30 mL/kg crystalloid fluids within 3 hours of sepsis identification.
- This recommendation is also part of the CMS SEP-1 compliance guidelines.
- The determination of 30 mL/kg is based on average fluid volumes administered in previous large sepsis trials.
- The topic remains controversial, with questionable mortality benefit.
- Additional studies demonstrate deleterious effects of large fluid volumes in critically ill patients.
- Patients with end-stage renal disease, heart failure or with advanced age often receive less fluids or have delays in administration with varying degrees of mortality impact.
- There is a paucity of high-quality data to guide clinical practice.
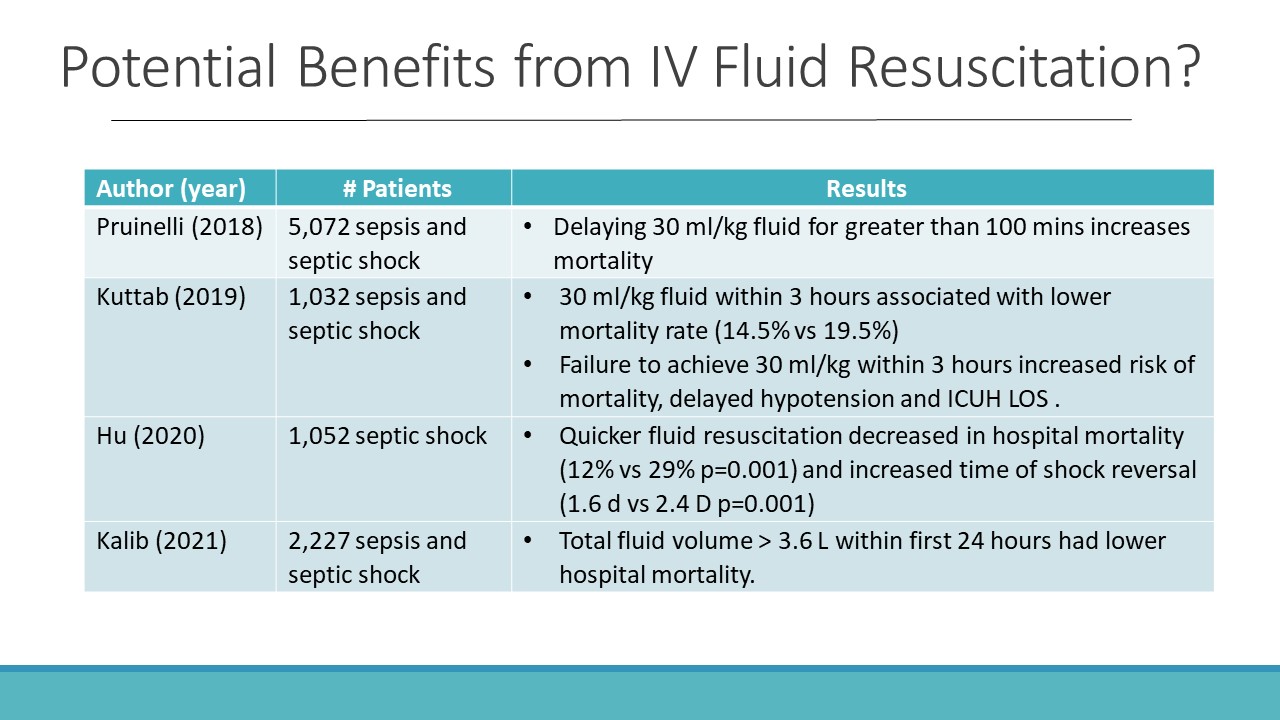
- Table 1 indicates several recent studies demonstrating a benefit to early IV fluid resuscitation.
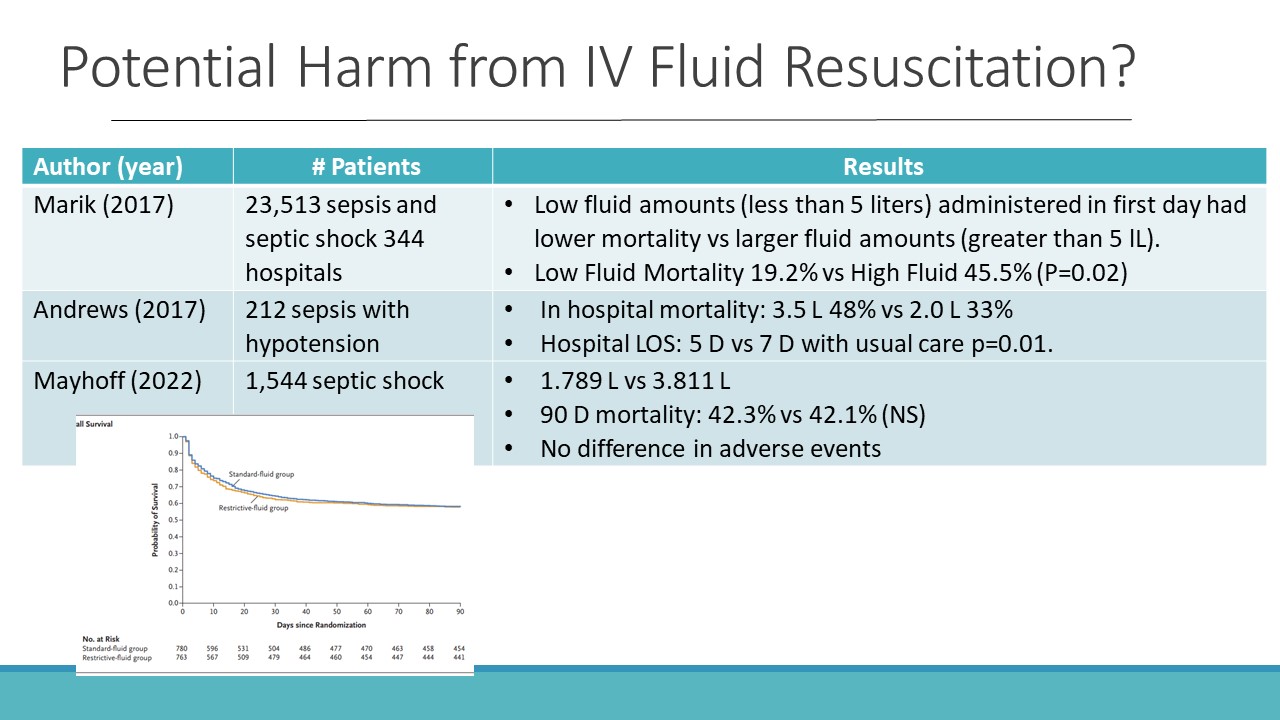
- Table 2 indicates several recent studies demonstrating limited value or even potential harm with IV fluid resuscitation.
- The significant heterogeneity of sepsis makes the generalization of a recommendation difficult.
- Key study weakness in both camps include:
- Small underpowered data groups
- Often single center studies
- High risk of methodologic bias
- Wide variances in therapeutic approaches to fluid administration
- Inconsistent outcome reporting
- Missing data
- Missing outcomes other than mortality and length of stay
- Well designed, large multicenter clinical trials are needed
- Plausible current approach:
- In patients with evidence of tissue hypoperfusion, fluid administration is most likely beneficial.
- If tissue perfusion appears satisfactory, fluid administration may not have a rational role
- When fluid administration has failed to improve hypoperfusion, earlier initiation of vasopressor therapy is associated with hemodynamic resuscitation and reduced mortality
CONCLUSIONS:
- Fluid resuscitation is not without potential harm and may be of questionable value.
- Clinicians should recognize the substantial heterogeneity of sepsis and focus on tailoring fluid resuscitation to the individual needs of the patient based on assessment of clinical responsiveness.
- Earlier use of vasopressors to fluid administration should be considered in unresponsive patients.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.