Early Restrictive or Liberal Fluid Management for Sepsis: The CLOVERS Study
SUMMARY
- Complete fluid resuscitation should consider macrovascular perfusion as well as microvascular perfusion.
- There is a lack of data to adequately guide clinicians on fluid and vasopressor use in early sepsis.
- The CLOVERS study suggests restrictive fluid with early vasopressor use or liberal fluid use resulted in similar patient outcomes.
REVIEW
- CLOVERS: Crystalloid Liberal or Vasopressors Early Resuscitation in Sepsis trial
- The goal of fluid resuscitation in patients with sepsis is to increase intravascular volume and improve organ hypoperfusion.
- For adequate fluid resuscitation, both macro vascular perfusion (stroke volume and cardiac output) as well as microvascular perfusion (capillary blood flow) should be addressed and corrected.
- Excessive fluid administration or vasopressor use have risks such as dilutive coagulopathy, fluid overload and pathogenic edema for the former, and tissue ischemia, increased cardiac work and arrhythmias for the later.
ANALYSIS of CLOVERS Study
- Multicentered, randomized, unblinded trial.
- 18 years old with suspected or confirmed infection with antibiotic administration and sepsis induced hypotension (systolic blood pressure < 100 mm Hg after 1L if IV fluid).
- Exclusion Criteria:
- > 4 hours hypotension
- Refractory to IV fluids of at least 1 litre
- > 24 hours after hospital presentation
- > 3 L fluid administered for this episode, including pre-hospital.
- Volume depletion from non-sepsis cause.
- Restrictive fluid strategy:
- Systolic BP < 100 mm Hg or MAP < 65 mm Hg after 1-3 L of IV fluids
- Up to 2 L additional fluid boluses allowed
- If MAP < 65 or SBP < 90 mm Hg, add norepinephrine
- Liberal fluid strategy:
- Systolic BP < 100 mm Hg or MAP < 65 mm Hg after 1-3 L of IV fluids
- Administer 2 L additional fluid over 180 minutes
- If hypoperfusion still exists, administer 500 ml bolus of IV fluid, repeat as needed
- Rescue vasopressor recommended for severe hypotension (SBP<70 or MAP < 50 mm Hg; Lactate > 4 or increasing; Clinical manifestations of fluid overload.
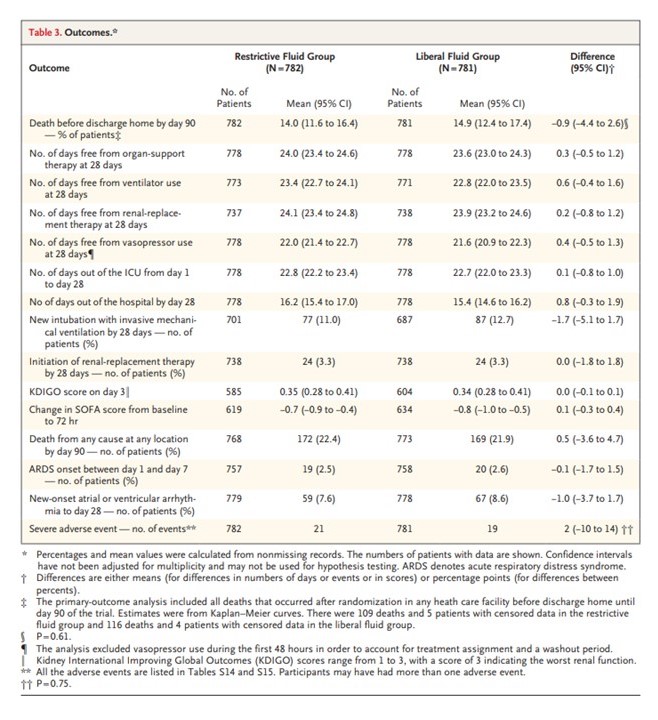
- Primary Outcome: Death by 90 days before discharged home
- Secondary Outcome:
- 28 day use of support (ventilator, renal replacement, vasopressor, days out of ICU and days out of hospital
- Safety outcomes: new onset respiratory failure; arrhymia; complications of catheter use.
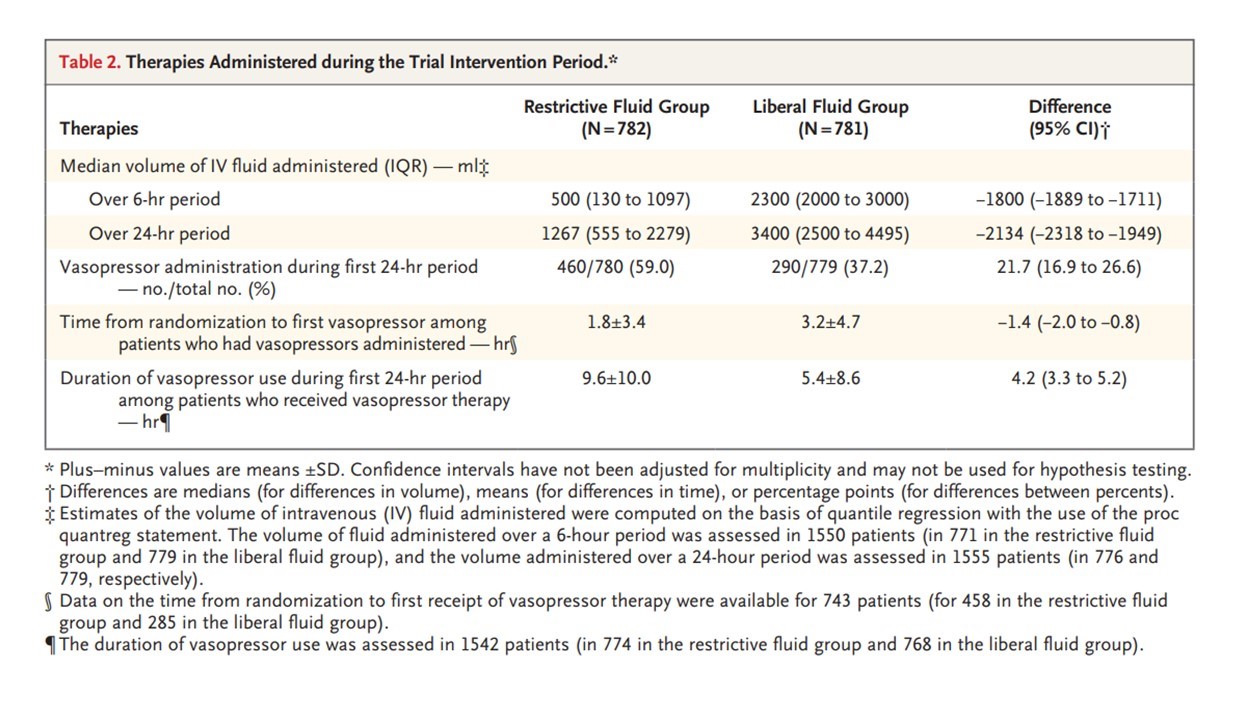
RESULTS
CONCLUSIONS
- Similar fluid administration prior to randomization occurred in both groups (~ 2L)
- Restrictive fluid strategy, with earlier vasopressor use, did not result in a difference (higher or lower) mortality before discharge home by 90 days than a liberal fluid strategy.
- There was no difference in the incidence of 28 day complications including ventilation free days, renal replacement treatment, vasopressor use, days out of ICU or Hospital, new onset arrhythmias, or complications from the use of peripheral or central venous catheter use by either fluid strategy.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.