The Confusing State of Sepsis Definition
SUMMARY
- There is large variability in incidence and clinical outcome (including mortality) in sepsis patients based on the definition used.
-
The differing definitions make it difficult for providers and health systems to:
- Evaluate outcomes such as Time-Zero, mortality and length of stay
- Implement quality improvement initiatives
- Compare results between sites using different locations
- Identify patients who meet clinical criteria but fail to meet regulatory criteria or vice versa
- The various approaches lead to much confusion.
BACKGROUND
- The lack of a “gold standard” definition to sepsis has resulted in a confusing state of multiple, rapidly changing clinical and regulatory possibilities.
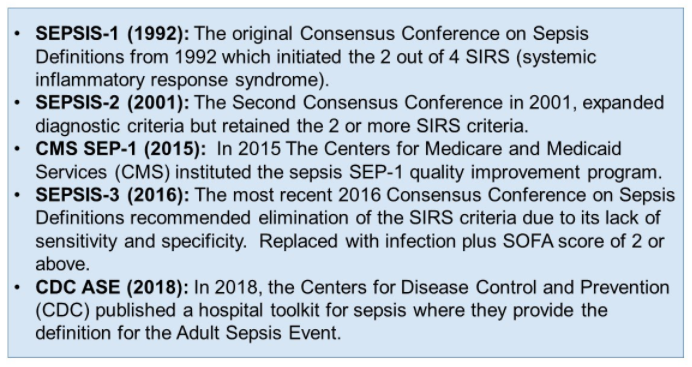
- Although the SEP-1 requirements have been amended twice, they retain the SEPSIS-2 2001 definition of 2 or more SIRS criteria coupled with the 2012 treatment recommendations from the Surviving Sepsis Campaign.
-
The result is a complex solution involving:a. Difficult to implement hospital sepsis quality improvement initiatives andcompare sites using different definitions.b. Hospitals supporting a robust data abstraction service to support SEP-1.c. Private insurance payers denying payment when documentation does not cite SEPSIS-3 2016 criteria.d. Some patients will meet both SEPSIS-2 and SEPSIS-3 definitionse. Other patients will meet only 1 of the definitions and get fully paid but failCMS SEP-1 criteria or vice versa
REVIEW
A recent retrospective analysis from Barnes Jewish Hospital/Washington University in St Louis, MO used hospital electronic medical record and administrative claims data to compare 5 different sepsis definitions. (Yu SC, Betthauser KD, Gupta A, et al. Critical Care Medicine 2021;49(4):e433-e443)
Six years of data were reviewed (2012-2017) which included 286,759 inpatient encounters.
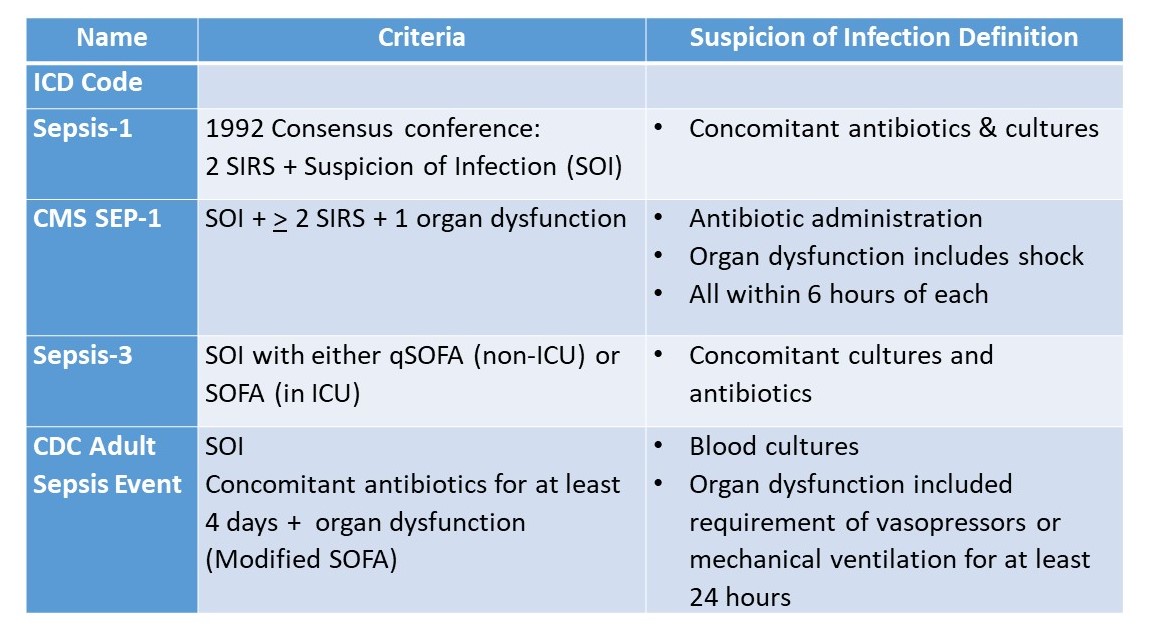
Table 1: Sepsis Definitions
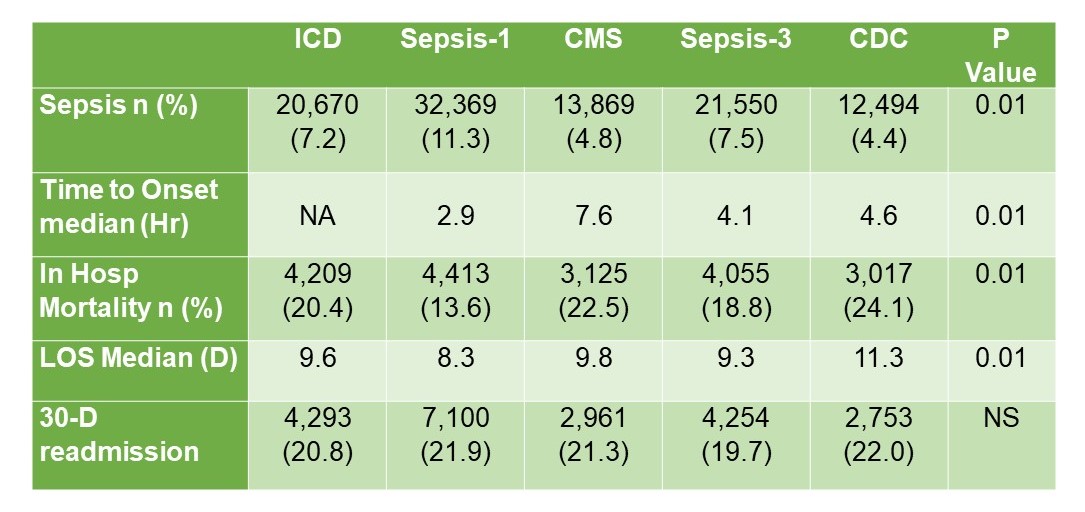
Table 2: Results of Differing Definitions
- Number of sepsis cases varies based on the definition used
-
- No singular definition captures the entire spectrum
- Only 4,370 cases met the criteria for all the definitions
- Time to onset varied as Time-Zero (T-0) definitions vary across the definitions.
- CMS SEP-1 had the longest time to onset due to the Time-Zero (T-0) definition used.
- T-0 for CMS SEP-1 is defined as the time the last point of the criteria is met.
- The CDC ASE had the highest mortality and length of stay, with one of the lowest incidence rates.
- A number of these definitions included sepsis and septic shock patients together
- Therefore, the true incidence of sepsis within this set cannot be determined.
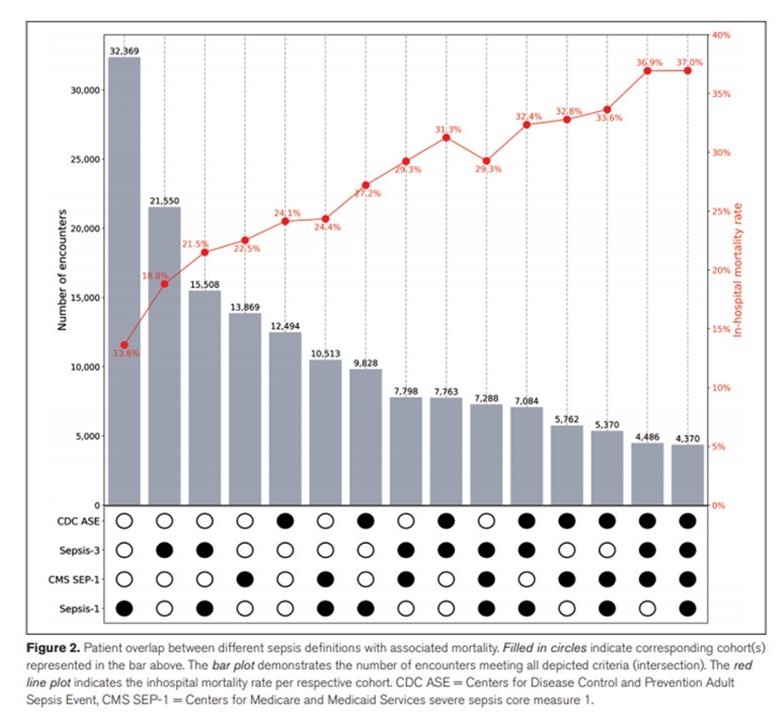
Table 3: Mortality Based on Definitions
CONCLUSIONS
-
Varying sepsis definitions lead to confusion.Hospitals and providers who target to meet CMS SEP-1 requirements, maybe denied payments by insurers based on more clinically oriented definitions (SEPSIS-3 or CDC ASE).
- Hospitals and providers who target to meet CMS SEP-1 requirements, maybe denied payments by insurers based on more clinically oriented definitions (SEPSIS-3 or CDC ASE).
- A more consistent list of criteria for sepsis definition is required.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.