Roadmap to a Successful Sepsis Quality Improvement Program
Quality improvement programs (QIP) on sepsis typically focus on early detection and treatment. These programs have demonstrated various approaches to protocol based therapy and “Sepsis Teams” functioning similar to rapid response teams are effective at sepsis bundle compliance and patient outcomes. However, it is unclear which specific components of a QIP provide the greatest impact on patient outcome. Also, there is a need to determine if a QIP will improve the Centers for Medicare & Medicaid Services (CMS) SEP-1 core measures.
Damiani et al reviewed 50 observational sepsis QIP studies. Although there was high inconsistency between the studies, overall, the studies did result in a statistically significant increase in sepsis resuscitation bundle compliance. The greatest increase in bundle compliance occurred in:
- Patients with higher illness severity indicative of risk of death
- Sites with low initial compliance with the bundle elements
- Teaching vs non-teaching hospitals
Mortality rates were also highly inconsistent, but the majority of studies demonstrated a significant decrease in mortality with QIPs.
Types of QIP components vary from pure educational programs (consisting of lectures, meetings, bedside trainings and various education materials) to specific process interventions aimed at decreasing the variability of care (examples include predefined order sets, clinical decision support, various screening tools).
Education alone and process change alone were able to improve bundle compliance and mortality. However, the largest improvement in bundle compliance and survival benefit occurred with the combination of both education and process QIP’s.
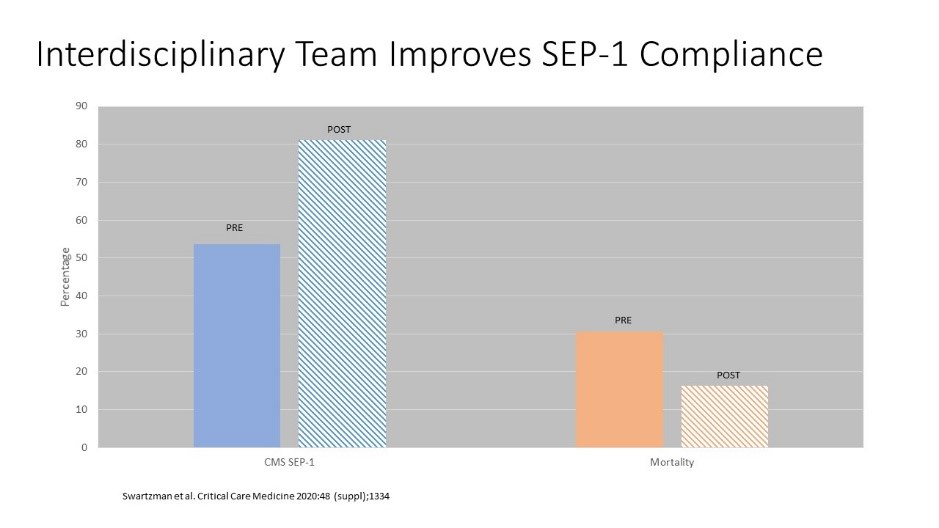
At the upcoming Society of Critical Care meeting, Christine Swartzman will present the impact of an interdisciplinary team QIP on the CMS SEP-1 core measures. The team developed a sepsis alert process and corresponding checklist for evaluation in the emergency department (ED) and inpatient areas involving the rapid response team. SEP-1 compliance improved from 53.6% to 81.1% associated with septic shock mortality dropping from 30.6% to 16.3% (Figure).
A hospital wide, standardized, interdisciplinary QIP for sepsis and septic shock is associated with improved bundle compliance and mortality outcomes. The best results are observed with a combined educational and process improvement QIP.
When it comes to sepsis, an effective Quality Improvement Program must address multiple practice areas, consisting of the ICU, ED and floor staff and patients. To ensure sustainable results, regular auditing of all patient data should occur along with feedback on the Quality Improvement Program’s results.
Damiani E, Donati A, Serafini G. et al. Effect of performance improvement programs on compliance with sepsis bundles and mortality: A systematic review and meta-analysis of observational studies. PLOSONE|DOI:10.1371/journal.pone.0125827 May 6,2015.
Swartzman C, Isaak S, Farooq O, et al. Interdisciplinary sepsis resuscitation process improves SEP-1 compliance and decreases mortality. 49th Society of Critical Care Medicine Congress. 2019. Critical Care Medicine 2020; 48 (1 suppl): A1334
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





