Evaluation of Risk Adjustment on Hospital Sepsis Mortality
SUMMARY
- The lack of a validated sepsis risk adjustment tool does not allow for a comparison of clinical outcomes across sites.
- Risk adjustment allows the evaluation of additional improvements such as identifying best practices, areas for improvement.
- A recent risk adjustment tool has been validated which should be used when comparing hospitals by sepsis mortality rates.
BACKGROUND
Comparing patient outcomes across sites without appropriate risk adjustment can be misleading.
Current sepsis measures tend to focus on compliance with time-sensitive processes (i.e. sepsis bundles or SEP-1 endpoints) rather than outcomes. Previous studies report raw sepsis mortality outcomes are measured based on:
- Administrative data which demonstrates large variability due to coding practices based entirely on patient demographics, comorbidities and coded illness markers
- Electronic health record data extracting, treatments, site of infection organ dysfunction and comorbidities.
Currently, existing mortality prediction models (APACHE, SAPS, etc) may not be appropriate for sepsis risk stratification due to limited granularity, variable accuracy, infrequently available measured clinical parameters, and electronic data in an unstructured format.
A validated, reliable risk adjustment is needed to benchmark and compare hospital sepsis mortality rates.
REVIEW
Recently, Rhee et al developed and validated a risk risk-adjusted for sepsis.
The primary endpoint for the model was in-hospital mortality for sepsis among patients meeting sepsis definitions during hospitalizations (Sepsis-3 criteria).
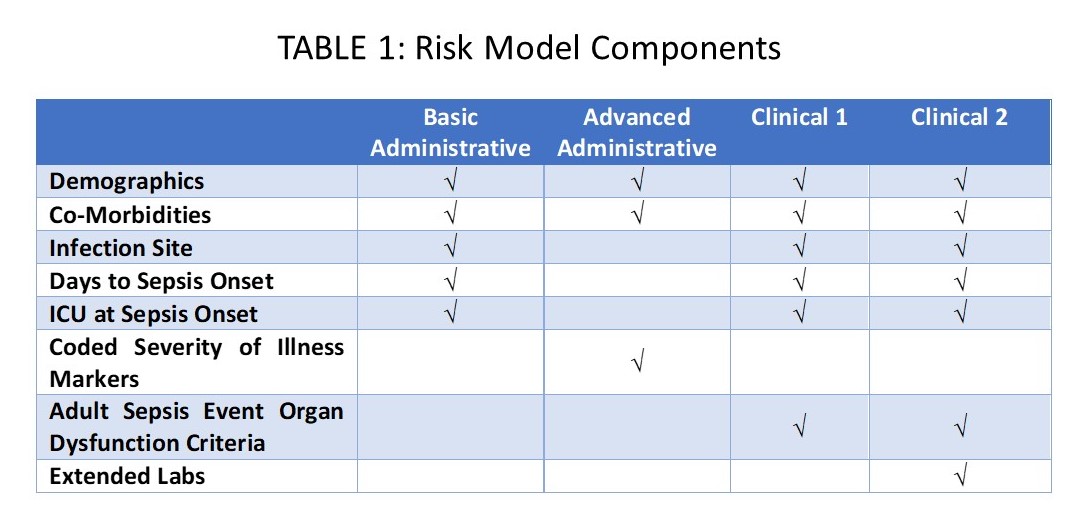
The risk model had 4 versions developed (Table 1):
- Basic Administrative model
- Advanced Administrative model
- Clinical model 1
- Clinical model 2
Models were Administrative vs Administrative plus Clinical segments
Model Development and Validation (Table 2)
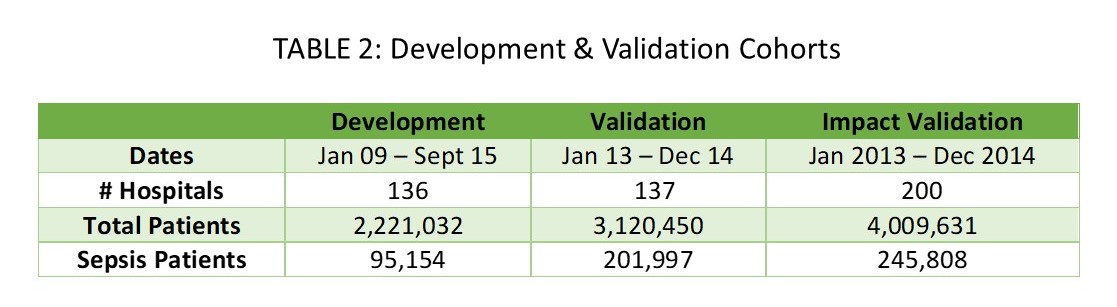
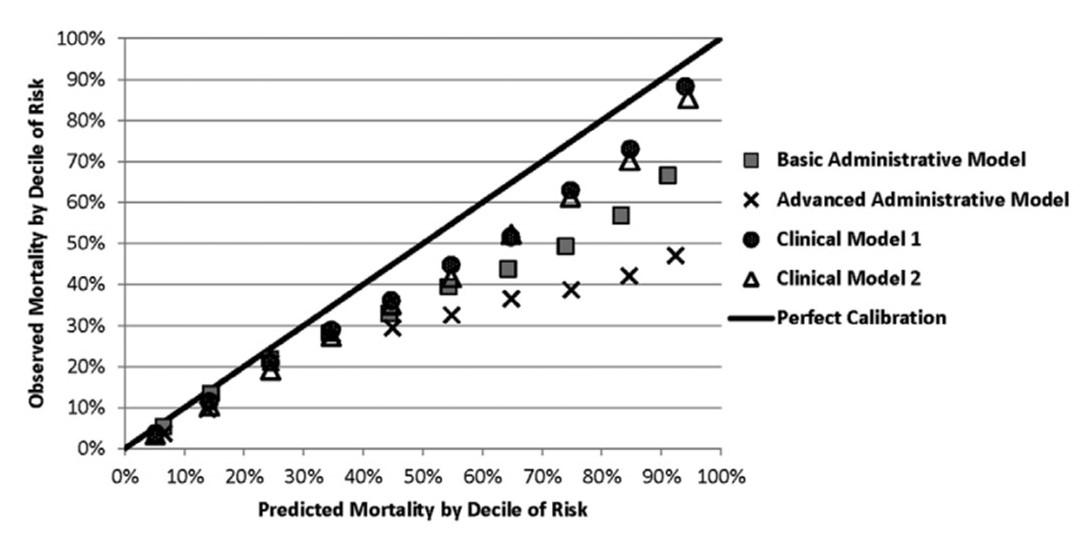
- The model based on clinical data elements substantially improved mortality predictions over administrative models alone. (AUC 0.82), Figure 1 & 2
FIGURE 1: Development Model Cohort
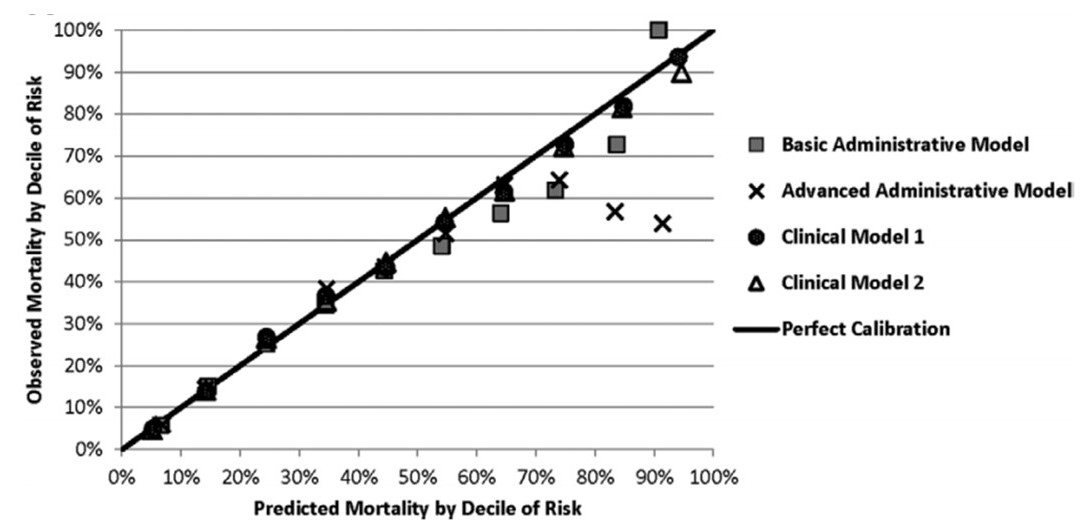
FIGURE 2: Validation Cohort
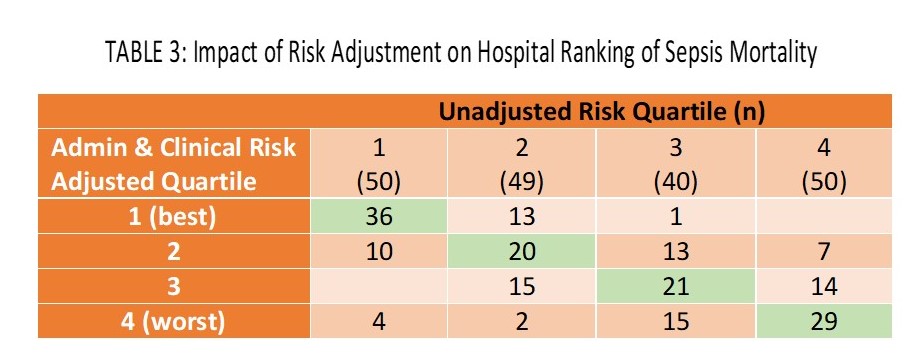
- The impact of the clinical model risk adjustment had a large effect on rankings of hospitals on sepsis mortality.
- A large number of hospitals shifted from the worst quartile into an improved quartile with risk adjustment (Table 3).
CONCLUSIONS
- Developing a risk adjustment for sepsis mortality provides the ability to compare in hospital mortality between hospitals.
- Incorporating clinical data with administrative data substantially improves the rankings.
- This model offers the first fully validated approach to sepsis mortality risk adjustment evaluations.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.