The Changing Definition of Sepsis in Clinical Practice
SUMMARY
-
There is no gold standard to the definition of sepsis
-
International conferences have evolved the definition of sepsis since 1991 by combining non-specific physiologic and laboratory abnormalities.
-
These conferences as well as the Centers for Medicare and Medicaid Services (CMS) offer clinicians various sepsis definitions.
BACKGROUND
Most clinicians agree there is no single, clear definition of sepsis in clinical practice.
In addition, treatment is often started later than desired, potentially minimizing optimal outcomes.
Since 1991, there have been 3 consensus conferences and subsequent publications in an attempt to define sepsis. Each conference has attempted to update and evolve from the last as new evidence is published in the field. At least 10 years has lapsed between the consensus meetings (Sepsis – 1: 1991; Sepsis – 2: 2001; Sepsis – 3: 2016).
The review below will highlight the conclusions of each consensus conference as well as some concerns.
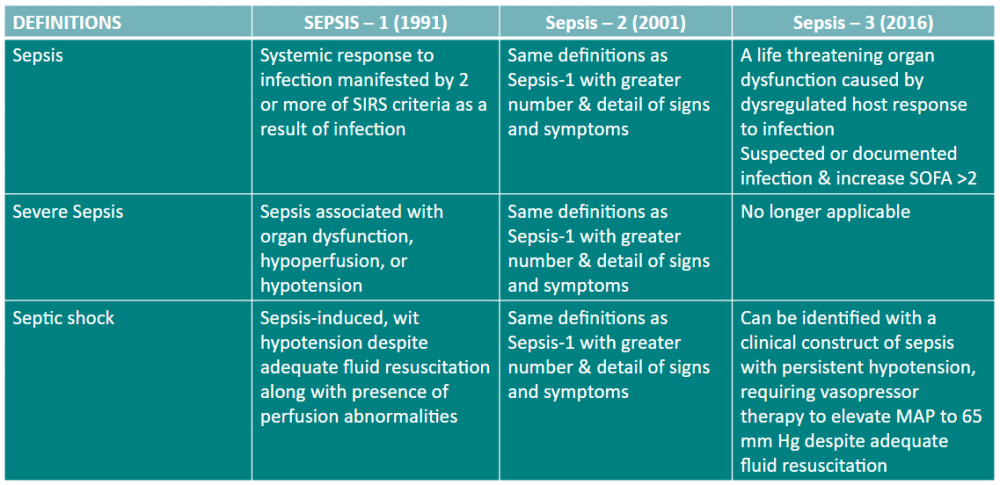
(Table 1)
REVIEW of Sepsis Definitions
Sepsis – 1 (1991)
The original consensus conference defined sepsis as a continuum of ongoing processes from sepsis to severe sepsis to septic shock.
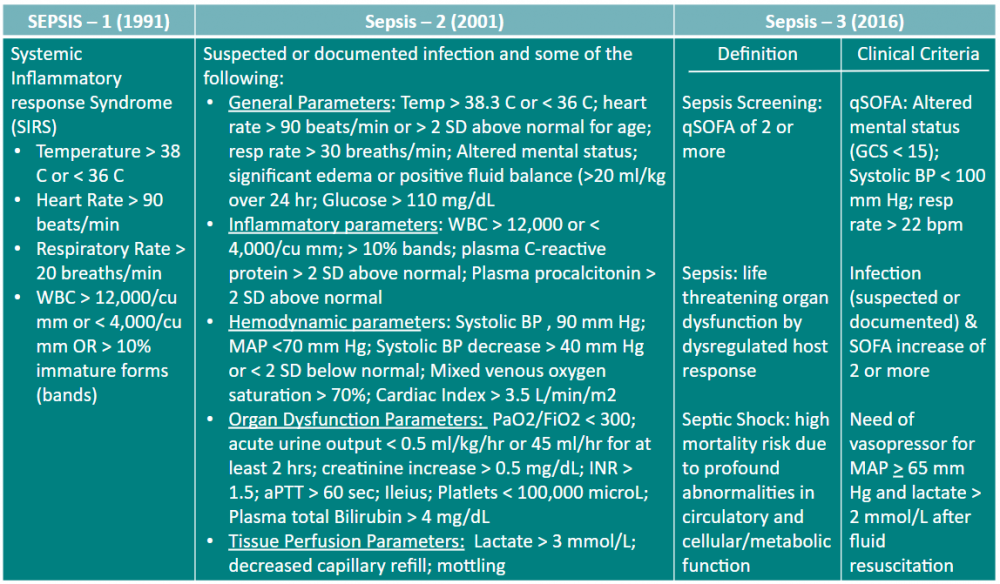
The basic component was the initiation of a systemic inflammatory response syndrome referred to as SIRS.
- Sepsis was identified as 2 or more of the 4 SIRS elements (Table 2) in addition to a known or suspected infection.
- Severe sepsis was defined as all criteria meeting the sepsis definition along with at least one organ dysfunction, hypoperfusion or hypotension.
- Septic shock was defined as the clinical situation where the patient was resistant to fluid and vasopressor therapy.
Concerns related to Sepsis – 1 definition
- SIRS are non-specific findings and may occur with numerous conditions, therefore not a sensitive indicator.
- Although the SIRS criteria are easy to remember, they use absolute cutoff values, i.e. a temperature above 38 C. Since sepsis is an “ongoing process” it is not rational to conclude a patient with a temperature of 39.9 C is more or less sick than a patient with a temperature of 38.1 C. However, only the latter value would contribute to a positive SIRS finding.
(Table 2)
Sepsis – 2 (2001)
For the Sepsis – 2 definition the diagnostic criteria from Sepsis – 1 were kept intact.
Severe sepsis was defined as “sepsis complicated by organ dysfunction”. This led to confusion toward the definition of sepsis and severe sepsis. With ten years of additional published data, signs and symptoms of sepsis were greater in number and detail.
These parameters were defined in order to help define the response of the patient with infection. Five areas were listed and defined as: General; Inflammatory; Hemodynamic; Organ Dysfunction; Tissue Perfusion (Table 2).
The original consensus conference defined sepsis as a continuum of ongoing processes from sepsis to severe sepsis to septic shock.
Concerns related to Sepsis – 2 definition
- Diagnostic criteria from Sepsis – 1 was kept in use
- Increased confusion with overlapping definitions between sepsis and severe sepsis
- Increased number of parameters difficult to use
Sepsis – 3 (2016)
New definitions were deemed necessary due to:
- low sensitivity and specificity of SIRS;
- to place greater emphasis on organ dysfunction; and
- advances in sepsis epidemiology and management.
Sepsis – 3 defined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection”.
Sepsis – 3 defines organ dysfunction as an increase of 2 or more in the Sequential Organ Failure Assessment (SOFA) score. SOFA score should be determined on admission and every 24 hours. In addition, a non-ICU bedside quick SOFA (qSOFA) score was developed for early identification of organ dysfunction of sepsis in these patients (Table 2).
Concerns related to Sepsis – 3 definition
- qSOFA is not a diagnostic criteria nor is it part of the Sepsis – 3 definition.
- The variation and trend in SOFA scores over time may be more important than a one time value
- SOFA score is outdated and needs to be updated
- The new definition does not allow for specific treatment based on the patient’s specific underlying cause of sepsis.
CONCLUSIONS
- Although the definition of sepsis has changed over the last 3 decades, there is still no gold standard definition.
- The lack of a standard definition will most likely continue until the definition moves from the current syndrome based terms to a biomarker based definition.
- Although easy to remember and use, SIRS has poor sensitivity and specificity
- Organ dysfunction may be due to causes other than sepsis. When infection is not certain with the presence of organ dysfunction, it is difficult to exclude the diagnosis of sepsis. This may delay early diagnosis and therefore therapy which is key to sepsis management.
Next week’s article will compare and contrast the evolution of the Sepsis Bundles (Resuscitation & Management) from 2004 to the current 2018.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.