Evolution and Current Status of Sepsis Bundles
SUMMARY
-
The Sepsis Bundles have been a key component to the implementation of the Surviving Sepsis Guidelines.
- The 2 different original resuscitation and management bundles have evolved over time both in terms of timeframe for completion and elements.
- There is unresolved controversy surrounding the newest 1-hour bundle elements and its appropriateness for bedside care.
BACKGROUND
The Surviving Sepsis Campaign (SSC) has been a joint collaboration of international critical care and infectious disease experts since 2002 with the goal of building awareness and reducing mortality of sepsis. Recommendations on the acute management of sepsis and septic shock were originally published in 2004. Subsequent revisions have been published in 2008, 2013, and 2017. Each revision is an update to the previous version as new evidence becomes available.
Although published separately from the SSC guidelines, the sepsis bundle elements have played a major role in the implementation of the guidelines. A bundle is a set of individual, evidence-based care elements which provide a greater proven benefit when applied together than individually.
REVIEW of Sepsis Bundles
2005 Bundle Definition
The original set of sepsis bundles consisted of a resuscitation (5 elements) and management (4 elements) bundle elements, to be completed within 6 and 24 hours respectively. From the beginning, several of these recommendations were questioned and not always accepted regarding their proven value.
While the 6 and 24-hour bundles were never tested prospectively, they remained part of the revised 2009 SSC guidelines.
The 2013 SSC revisions included revisions to the bundle elements after review of 32,000 patient charts from 239 hospitals in 17 countries. The management bundle was dropped. The resuscitation bundle was segmented into 2 parts: A 3-hour bundle (4 elements) and a 6-hour bundle (3 elements). The measurement of central venous pressure (CVP) and central venous oxygen saturation (ScvO2), without specific targets were recommended if the patient did not respond to fluid resuscitation. However, compliance with CVP and ScvO2 was highly variable and typically low, with their contribution to mortality reduction remaining questionable. Soon after these recommendations, additional data demonstrated the measurement of CVP and ScvO2 was not necessary for successful resuscitation and these elements were removed. However, in the presence of persistent hypotension or initial serum lactate concentrations above 4 mmol/L, some documented reassessment of intravascular volume status is required.
Following the 2018 SSC revisions, the 3-hour and 6-hour bundles have been combined into a single 1-hour bundle (5 elements). The goal is to begin both resuscitation and management immediately as longer delays may lead to higher mortality.
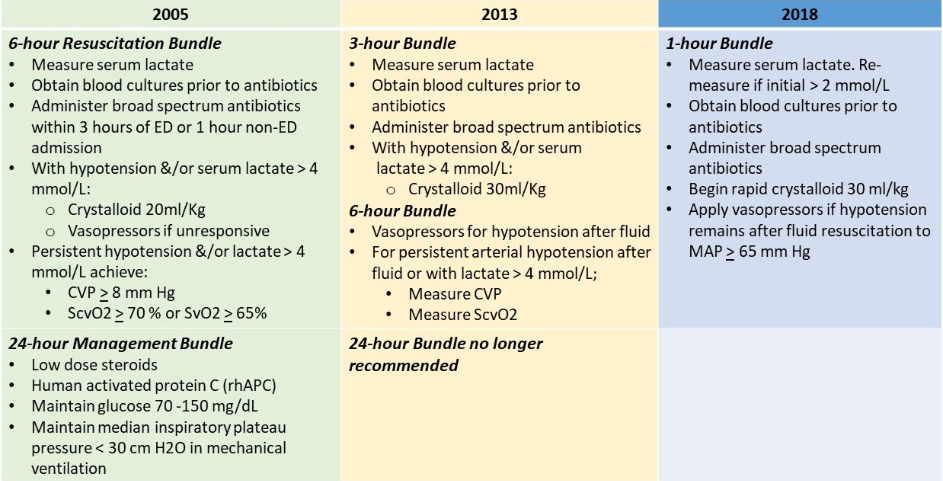
Table 1: Evolution of Sepsis Bundle
Apart from the administration of timely antimicrobials, controversy has erupted supporting the scientific evidence supporting the positive influence of these bundle elements on patient outcome.
- Large fluid volumes may be harmful to administer
- Measurement of serum lactate concentrations is unproven to improve patient outcomes
- A 1-hour target may over-diagnose patients with sepsis
- The Infectious Disease Society of America, Society of Critical Care Medicine and American College of Emergency Physicians do not endorse nor recommend the 1-hour bundle be implemented in the United States.
CONCLUSIONS:
- Bundles are intended as a tool to facilitate early diagnosis and treatment of the sepsis patient.
- The risk of death maybe higher in the beginning of the sepsis process rather than later, therefore, quicker onset of resuscitation and management may be warranted
- The 1-hour bundle timeframe may place undue burdens on clinical interventions and may not be feasible or beneficial
- A systematic individualized approach to the sepsis patient is preferred over a rigid set of mandated interventions.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.