Socioeconomic Impact on Sepsis
SUMMARY
-
Socioeconomic variables, beyond the control of patients and providers can impact the outcomes of sepsis patients.
-
Larger data sets are needed to confirm the full impact of socioeconomic factors on sepsis mortality and hospital readmission rates.
-
Further investigation to better understand socioeconomic variables on their influence to sepsis mortality is warranted.
BACKGROUND
-
Clinical outcomes are influences by a variety of factors including:
-
Demographics
-
Medical comorbiditiesIllness severity
-
Healthcare access
-
Hospital characteristics (i.e. teaching status, size, ownership, outcome metrics).
-
-
Social and environmental factors beyond the control of the patient plays a major role in driving health outcomes and can result in marked variations in health outcomes.
-
The most recent Surviving Sepsis Campaign recommendations (2021) include a best practice statement to screen for economic and social support as well as sepsis education for families and patients as they return home.
-
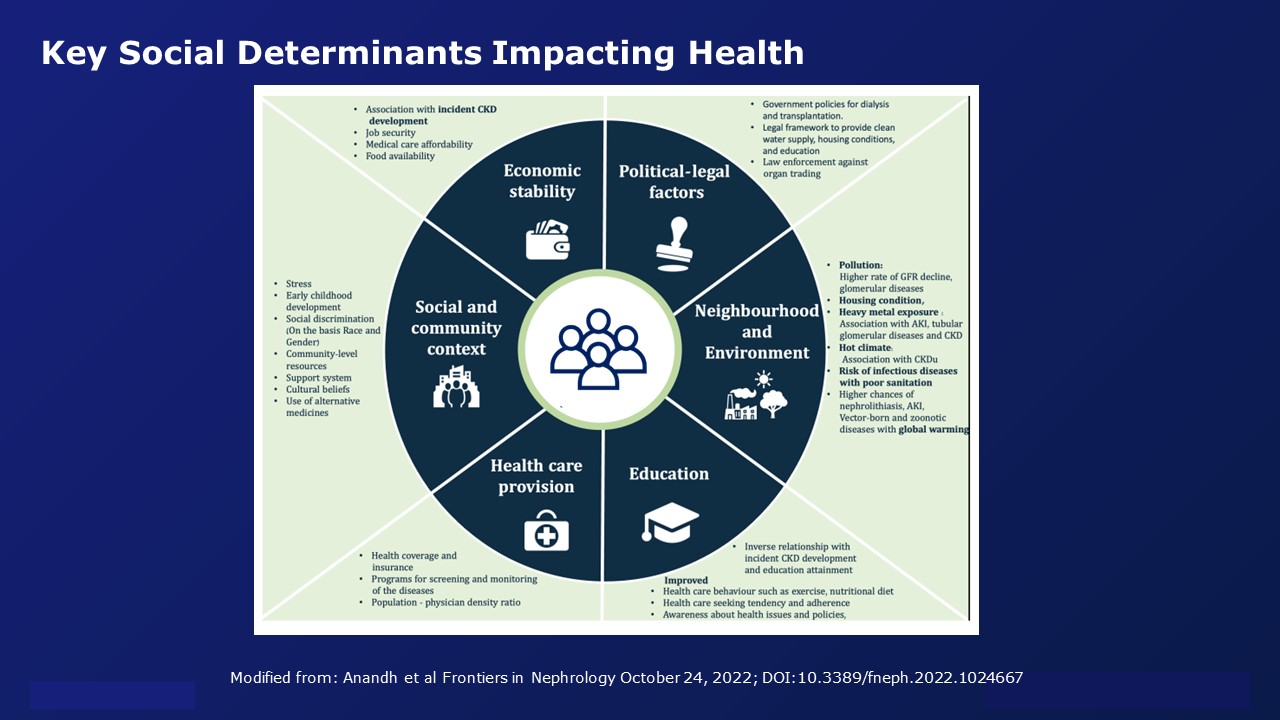
Key social determinants impacting health are illustrated in the figure:
Socioeconomic Determinants in Sepsis
-
Evaluating the effect of socioeconomic factors in sepsis has only recently been addressed.
-
It is unclear how social determinants effects the development and/or natural course of sepsis.
-
Key differences between studies are the definition used which demographically constitute a homogeneous community. Various methods used include:
-
Zip codes
-
County/City level data
-
Employment status
-
Insurance status
-
Education level
-
Age disparities
-
Area Deprivation Index (ADI – geospatial index of socioeconomic disadvantage)
-
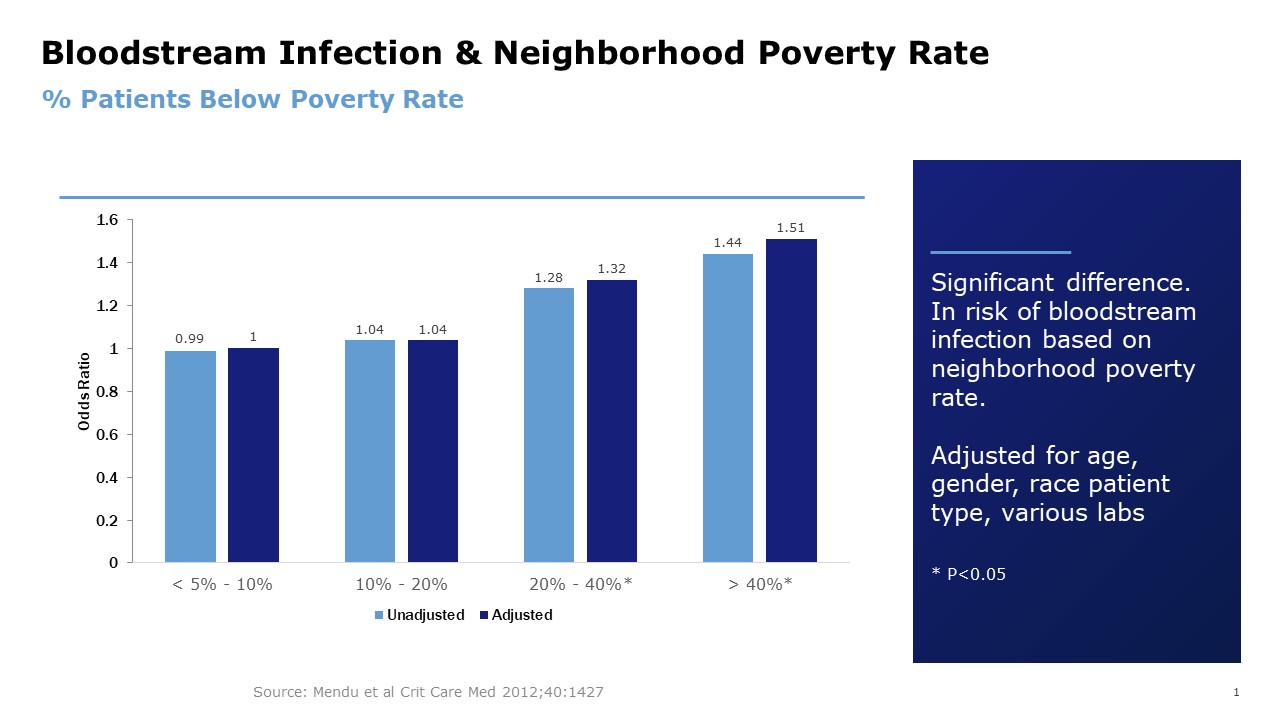
Bloodstream Infections
-
Although bloodstream infections occur in 0.5 to 1.3% of hospitalized patients, they are common causes of ICU admission with mortality rates from 20-40%.
-
14,597 patients had a bloodstream infection rate of 16.7% with 90 day mortality rates of 30.9% (Mendu et al Crit Care Med 2012:40:1427).
-
Neighborhood poverty rate was a strong predictor of risk of bloodstream infections.
Mortality
-
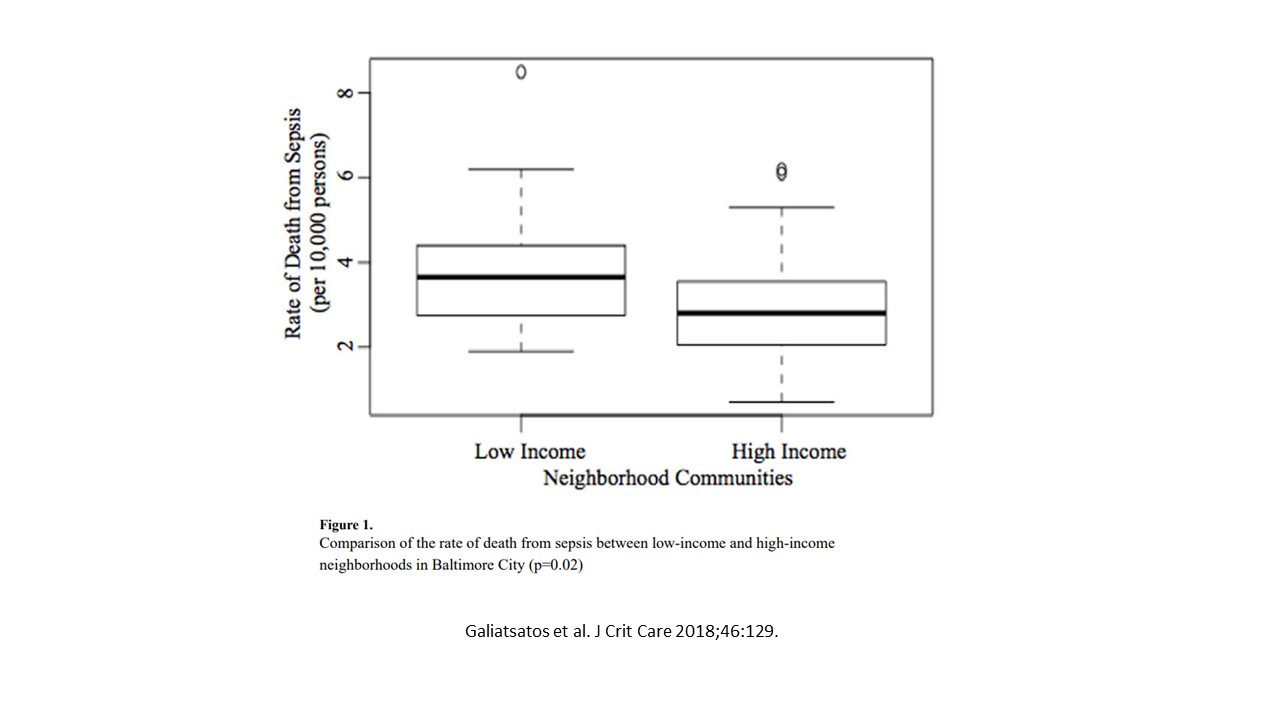
Lower income neighborhoods have a higher rate of sepsis attributable mortality than higher income neighborhoods (3.65 vs 2.80 per 10,000 persons, P=0.02)
-
55 neighborhoods in Baltimore City with median income (2015) $38,660. Low income at 25th percentile = $32,530. High income above 75th percentile $54,480.
-
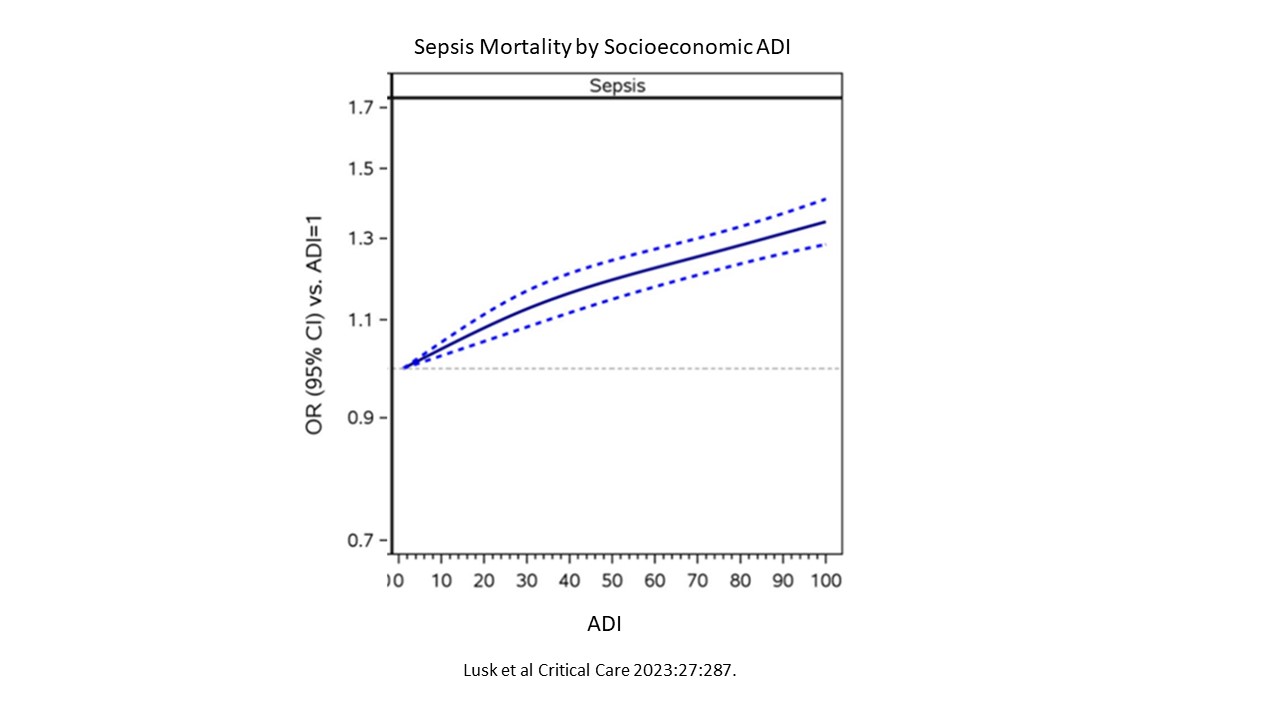
Lusk et al: 1,486,683 Medicare claims 2016-2019 admissions with DRG sepsis codes.
-
Neighborhood socioeconomic status via Area Deprivation Index (ADI).ADI is a measure of socioeconomic indicators (income, housing, employment, education).ADI scored from 0 (least deprived) to 100 (most deprived)
-
Sepsis mortality correlated with ADI
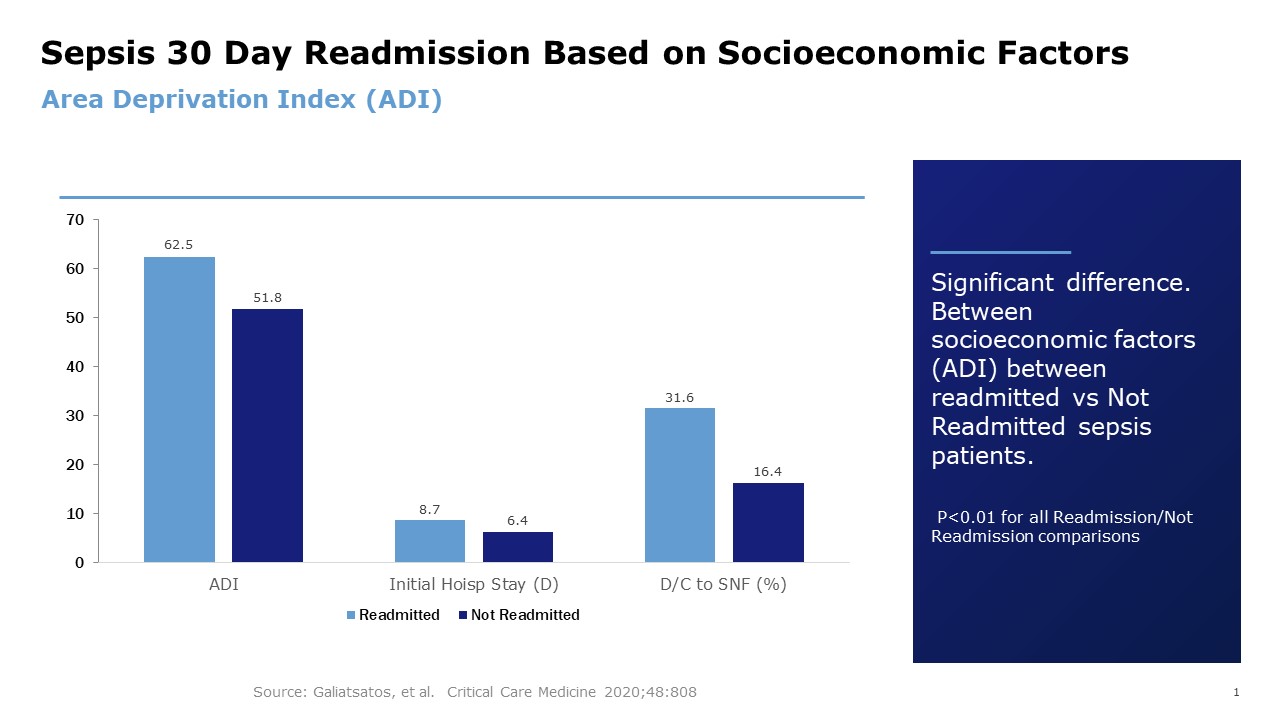
Hospital Readmission
-
ICD-10 codes for sepsis in 531 patients meeting Sepsis-3 definition
CONCLUSIONS
-
Socioeconomic factors are linked to sepsis outcomes in critical care.
-
Lower socioeconomic factors with sepsis have been associated with bloodstream infections, higher mortality rates as well as higher readmission rates.
-
Further investigation to better understand socioeconomic variables on their influence to sepsis mortality is warranted.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





