Should Hemodynamic Profiling be a Sepsis Best Practice?
SUMMARY
- Hemodynamic profiles in critically ill patients are complex and change over the sepsis course.
- Macro-circulatory and micro-circulatory factors contribute equally to the evolving disease state.
- During the later stages of hemodynamic impairment, both factors must be considered.
BACKGROUND
- In addition to source control and antimicrobial therapy, circulatory resuscitation is a key component of sepsis management.
- Hypotension and impaired end organ perfusion are primarily driven by macro-circulatory and micro-circulatory disturbances.
- Initially there is a linear relationship between macro-hemodynamics and end organ hypoxia. However, as sepsis progresses there is an uncoupling of:
a. Macro-circulatory and micro-circulatory systems
b. Micro-circulation and mitochondrial respiratory complexes. - With this uncoupling, maintaining macro-circulatory integrity alone (without considering micro-circulatory integrity), may not guarantee adequate tissue oxygen tension.
REVIEW
Macro-Circulatory Toolkit
- MAP is usually driven above 65 mm Hg, but this may not provide additional benefit
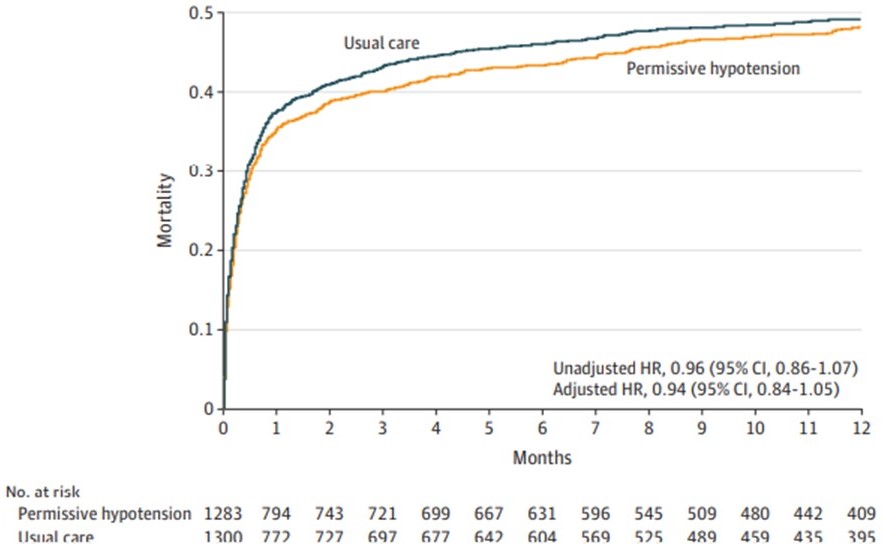
- Permissive hypotension (60-65 mm Hg) vs usual care demonstrated no difference in 90-day mortality.
Figure 1: Permissive Hypotension vs Usual Care MAP (Lamontagne et al JAMA 2020)
b. Cardiac Output Coupled with CVP
Provides parameters to fine tune fluid removal to match interstitial vascular fill rates
c. Tissue Perfusion
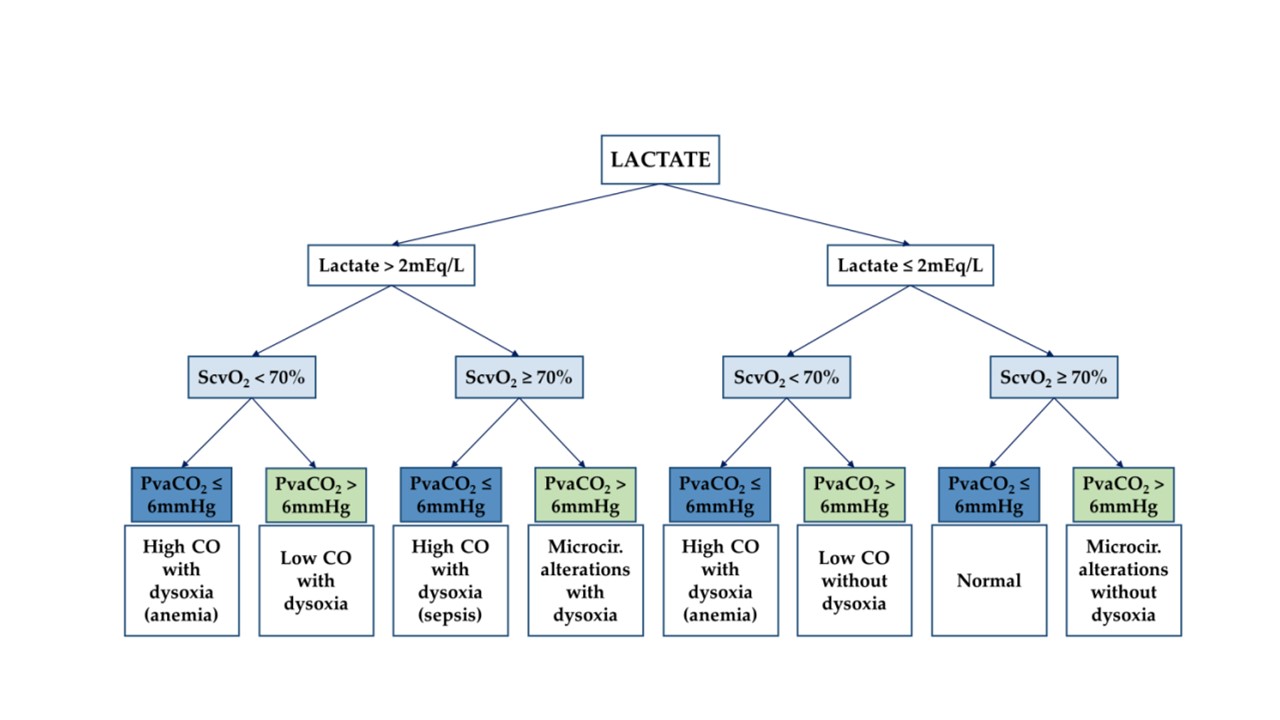
- Venous Oxygen Saturation (either central ScvO2 or mixed)
- Serum Lactate
- Carbon Dioxide Partial Pressure Difference (PvaCO2)
- Optimize these parameters to endpoints which identify and discriminate marco and micro-circulatory disturbances.
Figure 2: Hemodynamic Profile Optimization of Tissue Perfusion (Valeanu et al Diagnostics 2021)
d. Mean Systemic Filling Pressure (MSFP)
A stable MSFP can demonstrate optimal interstitial de-congestion with maintained cardiovascular stability
Micro-Circulatory Toolkit
a. 4 types of micro-circulatory alterations
- Complete circulatory arrest
- Decreased number of capillaries with continuous flow
- Complete circulatory arrest (Sepsis)
- Decreased number of capillaries with continuous flow (Sepsis)
b. Sublingual Micro-circulation Bed
- Represents micro-circulation disturbances in other organs
c. Tissue Oxygenation Based Parameters
- Several variables being evaluated:
i. Tissue carbon dioxide and oxygen (tPCO2 & tPO2)
ii. Tissue oxygen saturation (StO2
- Skin, via Capillary Refill Time (CRT) represents the best qualitative marker of impaired tissue perfusion.
i. CRT targeted resuscitation may result in less organ dysfunction than lactate targeted resuscitation.
CONCLUSIONS
- Strategies addressing macro- and micro-circulatory endpoints should be considered complementary to improve outcomes.
- Outcomes in the early stages of shock are primarily driven by macro-hemodynamics. However, in later stages, resuscitation should factor in micro-circulatory effects as well.
- A comprehensive hemodynamic framework combining macro- and micro-circulatory factors should be considered in the resuscitation efforts of critically ill patients.
- Further delineation of appropriate bedside applications is still needed.
Contact me to learn more about Sepsis treatment approaches.
If you would like to have this free monthly blog article automatically appear in your inbox, please subscribe here: http://eepurl.com/gFJKYD
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.