Sepsis Programs in Acute Care U.S. Hospitals
SUMMARY:
-
Sepsis programs within a hospital have been found to decrease:
- Mortality
- Length of stay
- Hospital costs
-
The National Healthcare Safety Network conducted a survey in 2022 acute care hospitals on their sepsis programs.
- Of 5,221 respondents, the majority of hospitals reported the presence of a sepsis committee with responsibility for oversight.
- Effectiveness of sepsis programs was not evaluated.
- Presence of programs and their features varied by hospital size.
- Opportunities exist for future enhancements.
REVIEW:
-
Survey about sepsis programs focused on:
- Leadership support for sepsis activities
- Approaches to rapid sepsis identification
- Sepsis management approaches
-
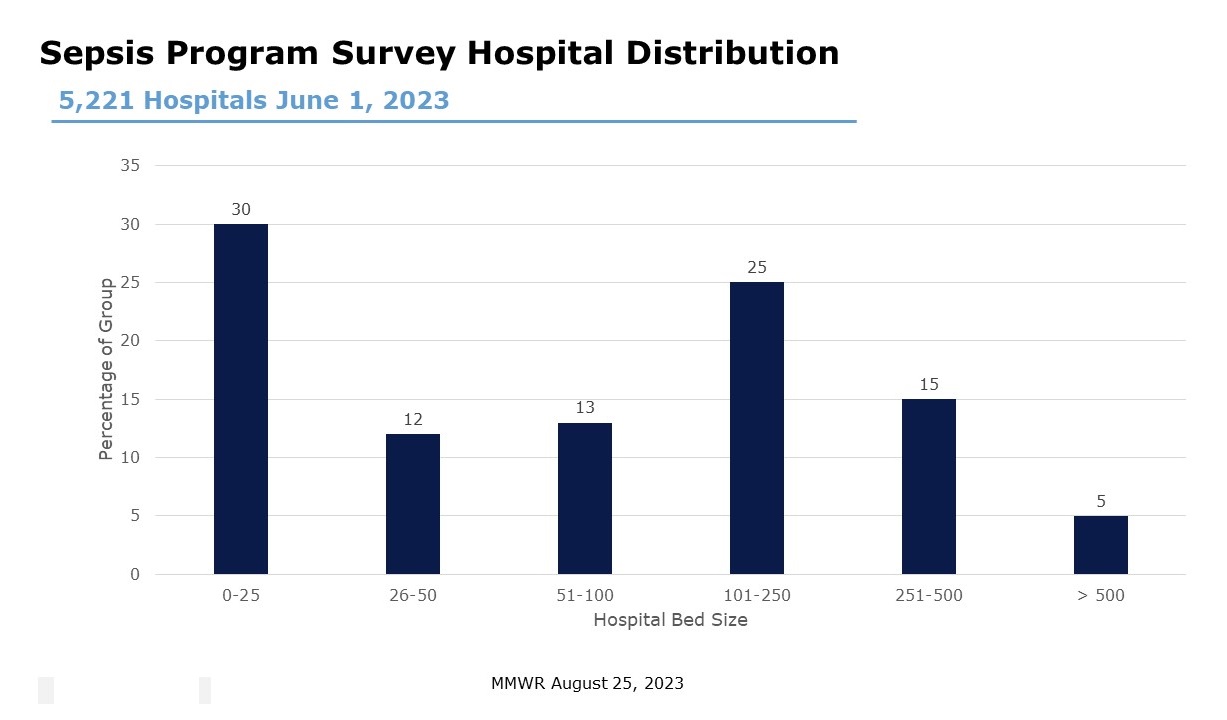
5,221 acute care hospitals responded
- The majority (55%) of respondents were smaller size hospitals.
- Very few large size hospitals responded.
EPSIS PROGRAMS:
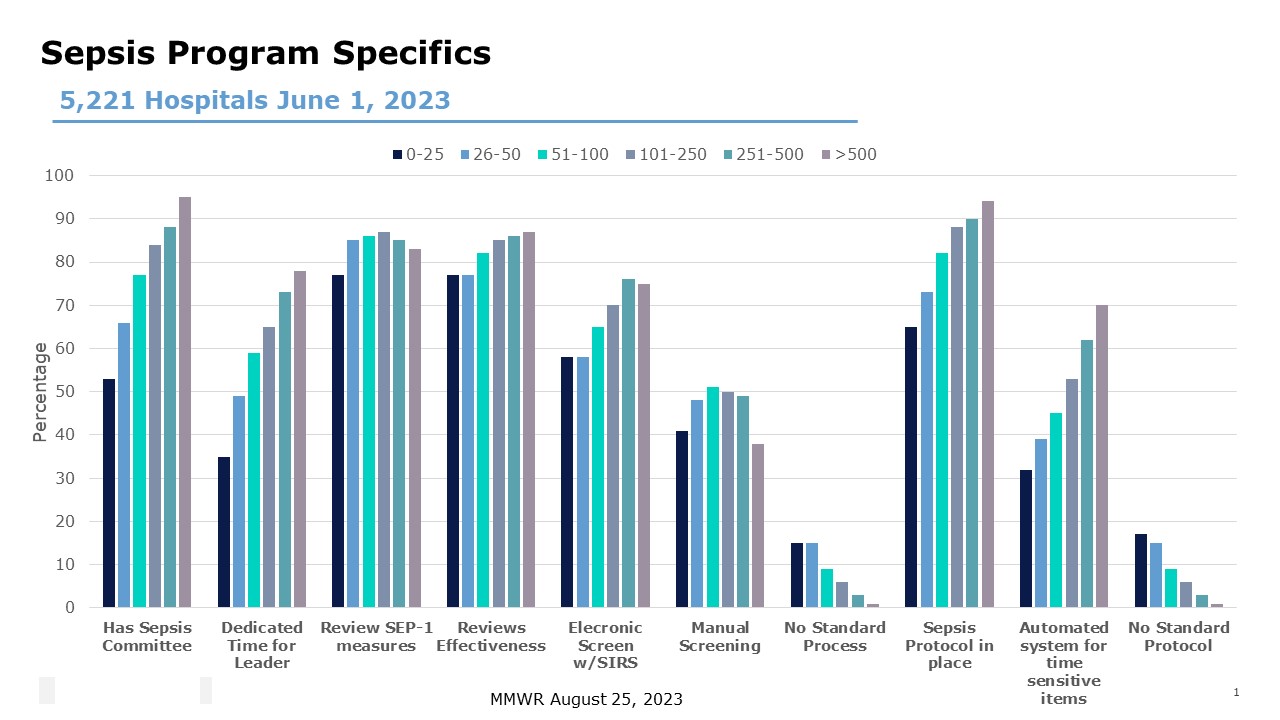
- Overall 73% of hospitals reported having a sepsis committees.
- Sepsis committees were less prevalent in smaller hospitals and progressively increased based on hospital size.
- Providing sepsis program leaders dedicated time as well as allocating resources to support sepsis efforts followed a similar trend.
- Review of CMS SEP-1 measures as well as monitoring and reviewing the effectiveness of sepsis strategies was a very common goal regardless of hospital size.
- Most hospitals had an EHR-generated sepsis alert based on SIRS criteria
- A small amount had a similar alerting mechanism based on qSOFA criteria
- Effectiveness of these programs is suspicious with 38 (large hospital) to 51% (101-250 beds) of hospitals having a manual screening process in place.
- Most hospitals reported having a sepsis protocol in place.
- However, mostly smaller hospitals do not have an automated system to prompt for the compliance of time sensitive aspects of sepsis care.
-
- This progressively increased from small to large hospitals.
CONCLUSIONS:
-
Self-reporting by hospitals indicates the prevalence of sepsis program committees.
-
The purpose of these committees is to monitor and review effectiveness of sepsis care within the hospital, however, definitions of a sepsis program was not required for this survey.
-
However, smaller hospitals appear limited in sepsis leadership, rapid identification and management practices as compared to larger hospitals.
-
This survey identifies opportunities to further improve the structure and care of the hospitalized sepsis patient.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





