Sepsis Performance Programs
Can Optimize Patient Outcomes
Can Optimize Patient Outcomes
SUMMARY
- Sepsis performance improvement programs can optimize compliance with sepsis protocols and are associated with improved patient outcomes.
- Having a Sepsis Performance Improvement program is more important than the specific content of the program.
- Engaging a large multidisciplinary group of clinical leaders is essential for success.
REVIEW
- Despite variances in Sepsis Performance Improvement Programs, they are consistently associated with increased bundle compliance.
- Although there are multiple components to a Sepsis Performance Improvement Program, the factors independently associated with improved bundle compliance and decreased mortality are:
- Use of Screening tools
- Workflow Process Changes
- Educational Programs
USE OF SCREENING TOOLS:
- The goal of sepsis screening tools is NOT to diagnose sepsis, but rather for early identification of possible sepsis cases requiring further evaluation.
- Sepsis screening alone will not result in improved performance measures or patient outcomes.
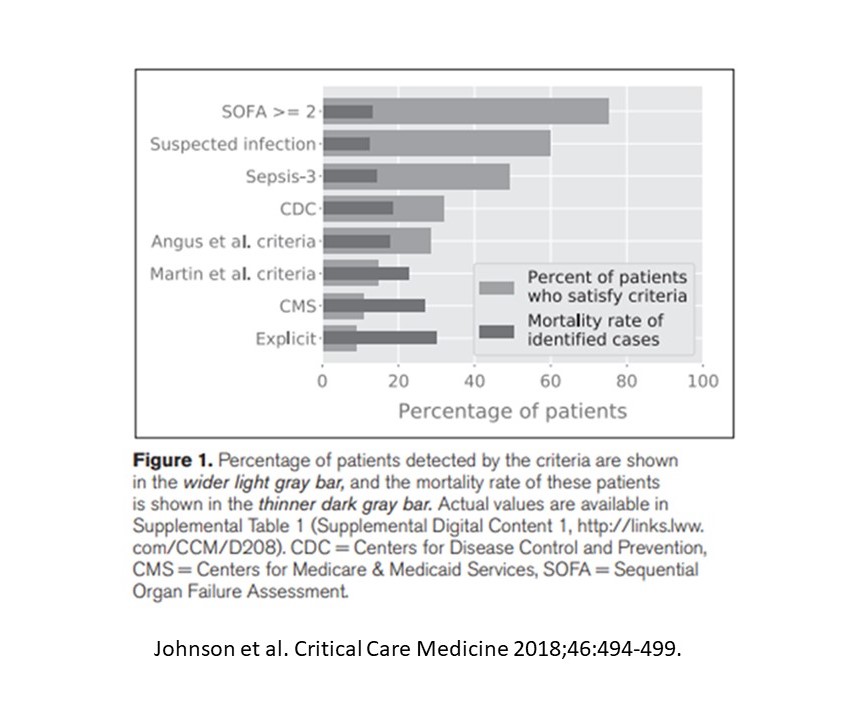
- A large number of risk scores and screening tools are available (SIRS, MEWS, NEWS, qSOFA)
- None are superior to any other
- Accuracy of the tools are highly variable
- All are susceptible to false positive findings
- Artificial intelligence may help improve the value of these tools.
WORKFLOW PROCESS CHANGES:
- Once a suspected sepsis patient has been identified, implementation of the response is the most critical step.
- Dedicated teams to respond to sepsis alerts, prevents placing the full burden of responsibility on a single extremely busy individual.
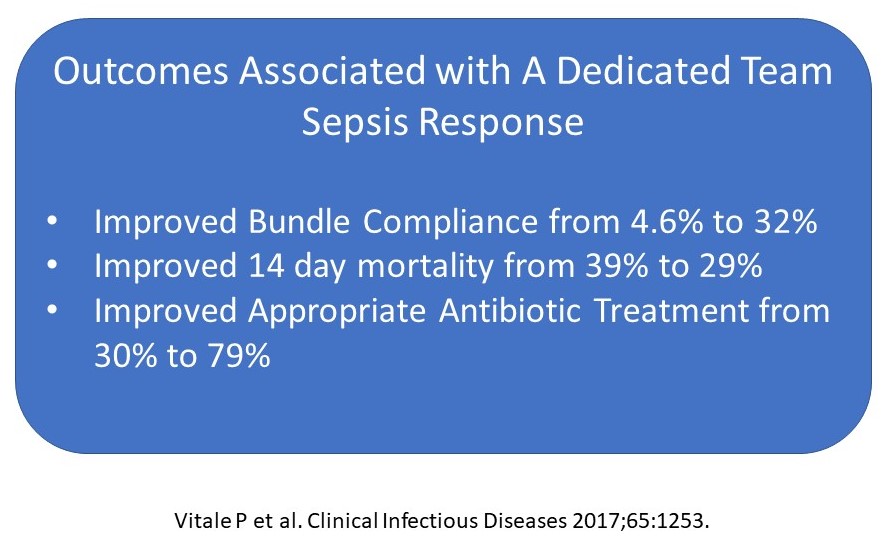
- The use of a dedicated team has proven improved clinical outcomes.
- Other process changes contributing to better bundle adherence include:
- Printed/easily accessible protocols
- Standardized order sets
- Frequent auditing
- Nurse driven protocols
EDUCATIONAL PROGRAMS:
- Increased awareness of the sepsis approach via an educational program is essential.
- Education materials could consists of:
- Lectures
- Bedside teaching
- Simulation training
ADDITIONAL CONSIDERATIONS:
- It remains to be seen if improved patient outcomes are due to:
- Care bundle adherence
- If 1 bundle element is of greater value than any other
- If increased awareness irrespective of bundle adherence is important.
- Should we be considering other endpoints than mortality, such as:
- Resource use
- Duration of invasive treatments
- Development of organ dysfunction requiring high levels of care
CONCLUSIONS:
- Implementing a Sepsis Performance Improvement Program is associated with a number of improvements in care processes and patient outcomes.
- Dedicated sepsis teams increase collaborative and timely discussions.
- Workflow changes allow incorporation of clinical judgement while applying the recommended elements of sepsis care.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





