Sepsis Clinical Probability Determination and Antibiotic Timing
SUMMARY
- Accurate diagnosis of sepsis upon presentation is challenging due to subtle disease presentation or rapidly progressing symptoms.
- Early administration of antibiotics is one of the most effective interventions, especially with severe disease, however, must be balanced with the risk of potential harm.
- Surviving Sepsis Campaign 2021 include antibiotic timing recommendations based on sepsis probabilities (Low, Possible, Probable and Definite).
REVIEW
- Patients are currently categorized as septic or non-septic upon hospital discharge.
- Interventions are then judged on what should have been done in retrospect.
- Sepsis programs should be evaluated if responses were appropriate based on probability of sepsis and urgency of disease state at time of evaluation.
- Sepsis diagnosis is based on clinical judgment, however, often the diagnosis is unclear, especially early in the patient’s presentation.
- Decisions to start antibiotics must often be made at a time when the diagnosis is still unclear.
- Early antibiotic administration is one of the most effective interventions which impact sepsis mortality rates.
- In patients with septic shock, each additional hour delay is associated with a 1.04 increase odds of in-hospital mortality.
- In patients with sepsis without shock, there is less consistent evidence between time to antibiotics and mortality.
- Performance measures encourage early antibiotic treatment.
- However, early intervention must be balanced against potential harm associated with unnecessary antibiotic administration to patients without infection:
- Allergic reactions
- Kidney Injury
- Antimicrobial resistance
PRESUMPTIVE SEPSIS PROBABILITY
- Surviving Sepsis Campaign 2021 outlined antibiotic administration timing based on the likelihood of clinical sepsis suspicion (Definite, Probable, Possible).
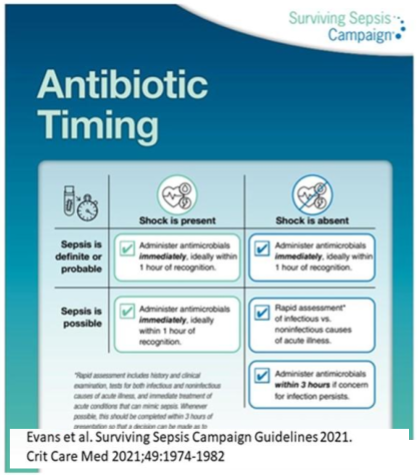
- Definite or Probable Sepsis or Sepsis with Shock: Antibiotics administered within 1 hour.
- Possible Sepsis without shock: Antibiotics administered within 3 hours with assessment of infectious vs non-infectious causes.
- Low likelihood of infection: Defer antibiotics with continued assessment for cause of acute illness.
- Recently Hooper et published a large analysis of 8,267 hospitalized patients evaluating the initial and final diagnoses of infection in patients meeting the Sepsis-3 criteria.
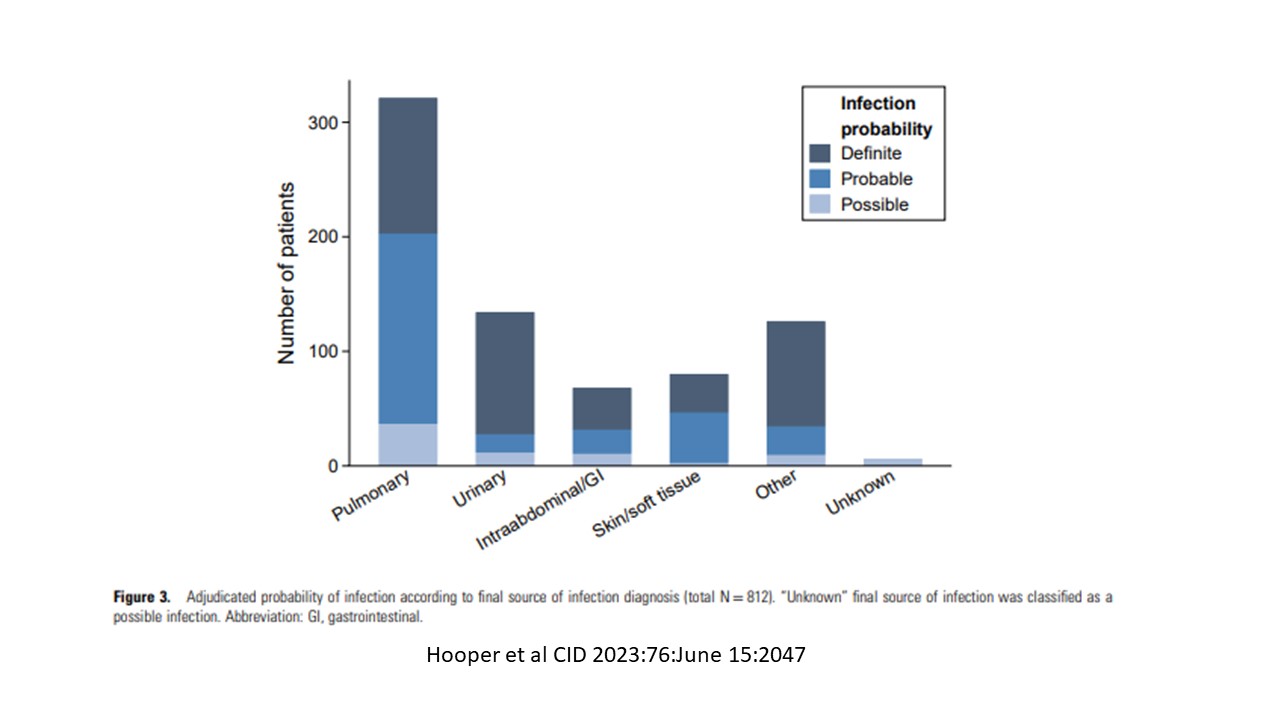
- 7 sources of infection: Pulmonary; urinary; skin/soft tissue; abdominal; unknown; other; not infected
- All patients were stated on antibiotics
- 699 (8.5%) were not infected (i.e. False Positives)
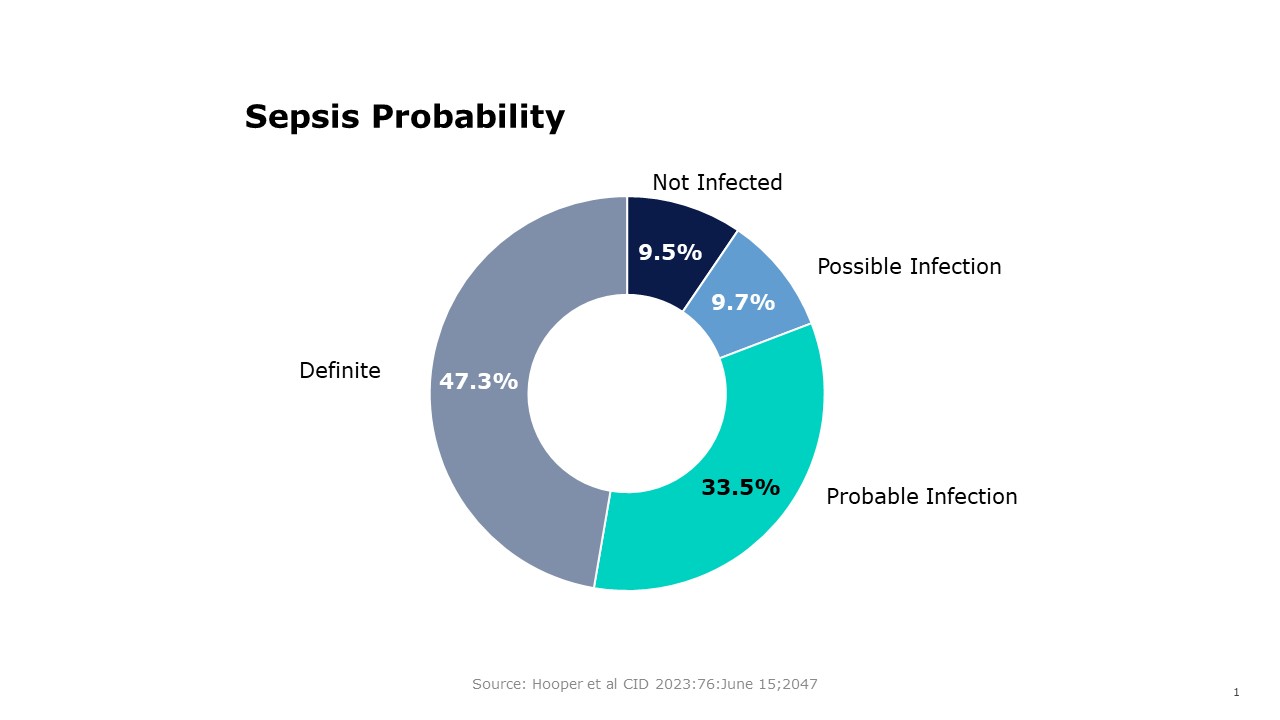
- A subset of 812 patients evaluated:
- 77 (9.5%) not infected
- 79 (9.7%) possible infection
- 272 (33.5%) probable infection
- 384 (47.3%) definite infection
CONCLUSIONS
- A large percentage of patients being evaluated for sepsis lave low or possible clinical probability.
- This percentage will most likely be site dependent.
- The timing of antibiotic prescribing should follow current recommended guidelines of 3 hours in this group.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.