Sepsis Associated Encephalopathy (SAE)
SUMMARY
- SAE is a key manifestation of sepsis occurring in up to 70% of ICU patients
- Associated with higher ICU and hospital mortality and long term consequences
- Difficult to assess, diagnose without specific treatment
BACKGROUND
- SAE is probably the most common type of encephalopathy in the ICU
- SAE may occur 36-48 hours BEFORE other systemic symptoms of sepsis.
- Therefore, should look for sepsis in any patient who develops changes in behavior or consciousness.
- Incidence approximated between 40-50% in sepsis patients
- Ranges reported between 8-70%
- Especially in patients with bacteremia
- No consistent definition of SAE
- Defined by a combination of extracranial infection with clinical signs of neurological dysfunction
- Clinical Manifestations range from impairment of awareness to delirium and coma.
- SAE is a diagnosis of exclusion
- Mental status changes may occur 36-48 hours before other systemic symptoms of sepsis
- Assess for sepsis in any patient with changes in behavior or consciousness
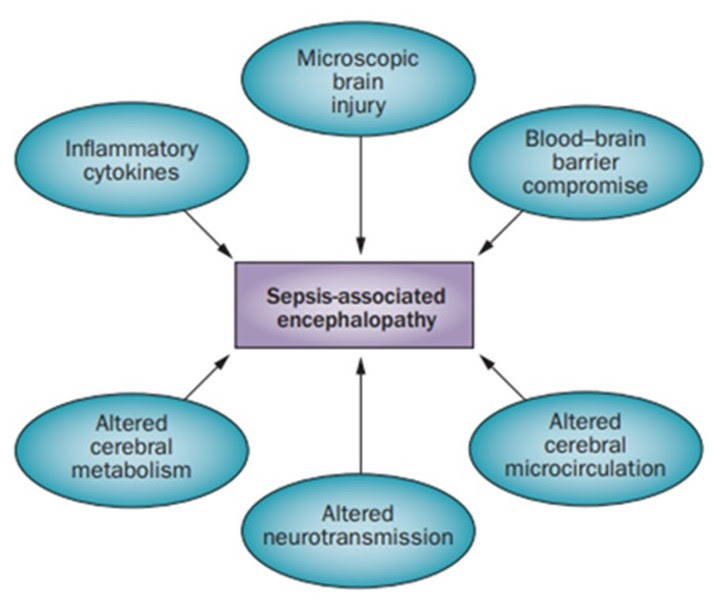
PATHOPHYSIOLOGY
- Molecular mechanisms leading to SAE not completely known.
- SAE probably multifactorial (Figure)
- Sub-divided into acute (Delirium) and chronic (Dementia) Phases
- Acute phase changes in patient consciousness
- Agitation, hallucinations, decreased concentration, coma.
- Delirium correlates with development of long term cognitive dysfunction
- Acute phase changes in patient consciousness
- Chronic phase dementia
- No exact risk factors identified contributing to poor neurocognitive outcome
- At discharge, between 45-62% of sepsis survivors have symptoms of long term cognitive dysfunction
DIAGNOSIS
- SAE is a diagnosis of exclusion
- Mental status changes in sepsis patients may be related to other causes than infection which should be assessed (i.e. electrolytes, vitamin deficiency, etc)
- Ensure primary cerebral pathologies are excluded
- Non-specific Findings:
- Cerebrospinal fluid
- Cerebral imaging (CT, MRI)
- Blood chemistries (CBC, electrolytes)
- Electroencephalograph (EEG)
- Abnormalities documented in 50% of sepsis patients
- Aids in assessing severity of SAE
- Non-convulsive seizures seen in up to 20% of cases
- EEG Grades & SAE

-
- Lack of strong correlation between clinical manifestations and EEG findings
- Screening: CAM-ICU or ICDSC is of great importance but infrequently used
- Risk Factors for SAE:
- Relationship between SAE & risk factors poorly related
- Possibilities include: Age; previous cognitive impairment; kidney or Liver failure; sepsis severity
TREATMENT APPROACH
- Patients with SAE have reported mortality rates up to 49% and greater than non-SAE sepsis patients (29%)
- The cause of the increased mortality is not knownNo specific treatment available
- Treat underlying sepsis
- There is a lack of evidence supporting treatment options are effective on SAE delirium
- Consider non-pharmacologic approaches: sleep; early mobilization; re-orientation, etc.
CONCLUSIONS
- Exact incidence, prevalence and mortality of SAE is unknown due to a lack of SAE definitive criteria.
- Probably the most common type of encephalopathy in the ICU
- SAE is a diagnosis of exclusion
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





