Optimal Antimicrobial Treatment Duration in Sepsis
SUMMARY
- There is limited guidance on the optimal duration of antimicrobial therapy for sepsis patients.
- Prolonged courses in severely ill patients is a common occurrence.
- With a lack of data, clinicians are left to consider a number of factors to define an adequate treatment course.
BACKGROUND
There is a surprising lack of guidance on the optimal duration of antimicrobial therapy for patients with sepsis. General recommendations, based on weak evidence, are for 7 to 10 days of therapy which may be lengthened or shortened based on clinical scenarios. However, over the past two decades, sepsis studies have not reported specific antimicrobial durations.
The optimal duration of antimicrobial therapy in sepsis is one that provides maximal clinical effectiveness while minimizing the associated risks, such as drug toxicity, C. diff associated disease, the emergence of drug resistance and health care costs. Prolonged courses of therapy are generally recommended to decrease the risk of relapse and to avoid the emergence of resistant organisms due to partial (and under) treatment regimens. However, the use of antipseudomonal beta-lactam use increases resistance by 4% for each additional day of administration.
Although recent trends have been to shorten antimicrobial treatment durations for a number of infections, there is a lack of data on the frequency, classes or duration of therapy is sepsis patients.
REVIEW
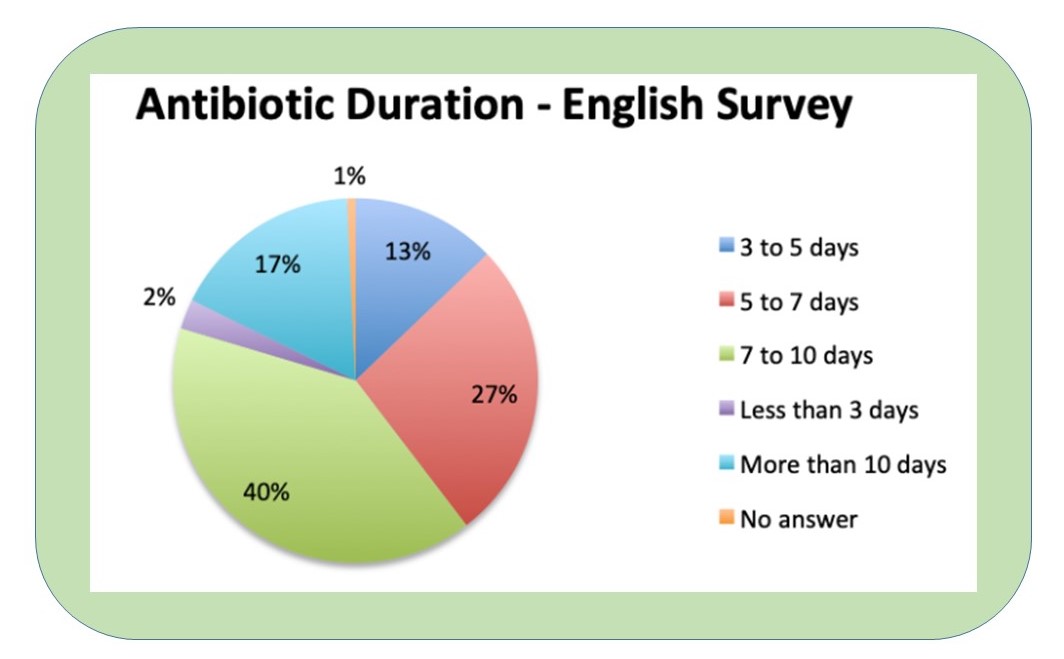
A recent survey of 265 practitioners from North America, Latin America and Europe report that 67% administer 5 to 10 days of antimicrobials in sepsis patients, with the majority at 7 to 10 days.
Major Factors for Consideration
1.SEVERITY OF ILLNESS
Patients are predisposed to longer durations of antimicrobial therapy with greater signs of clinical illness. Although there is not a clear association between severity of illness and the required length of therapy. However, providers appear to continue intravenous treatment based on illness severity.
Allowances are often given to patients demonstrating signs of clinical improvement before an ultimate duration is chosen. Admission to the ICU, hypotension, and acidosis are often associated with longer treatment durations.
2. CULTURE-NEGATIVE SEPSIS
A large portion of sepsis patients, and subsequently those receiving antimicrobials, will be culture-negative. Culture-negative sepsis patients tend to have longer antimicrobial therapy durations with no clear guidance for discontinuation.
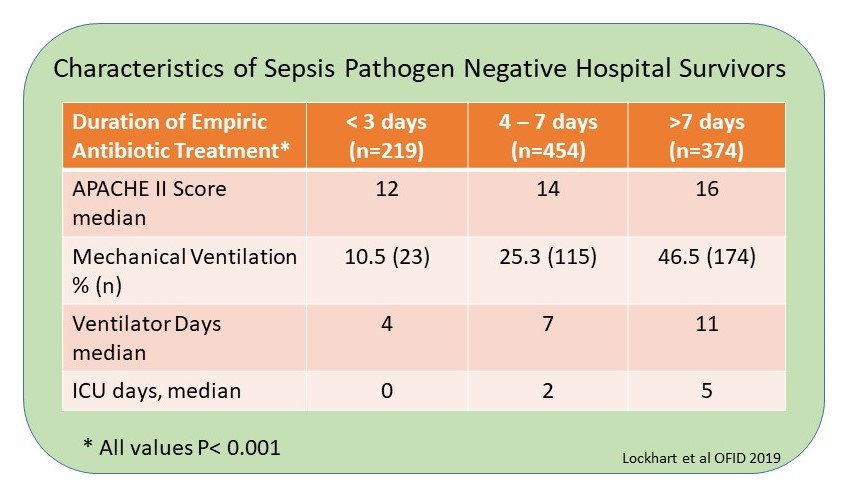
Culture-negative and severity of illness are tied together. A retrospective review from 2010-2017 of 1,047 sepsis survivors with pathogen negative cultures indicate duration of antimicrobial therapy is related to patient severity of illness.
3. SOURCE CONTROL
Patients with uncontrolled infection sites are typically excluded from trials evaluating shortened antimicrobial treatments. The inability to achieve infection source control is considered an acceptable indication for the extension of therapy duration.
4. MICROBIAL CHARACTERISTICS
Numerous organisms (i.e. Pseudomonas aeruginosa) present clinical challenges to eradicate. With limited guidance on optimal duration of therapy, providers typically opt for longer courses of therapy.
5. PHARMACOKINETIC/PHARMACODYNAMIC ISSUES
Critically ill patients pose a number of complex factors impairing reliable antimicrobial dosing to yield therapeutic drug concentrations at the site of infection.
These include:
- Altered renal blood flow
- Organ dysfunction
- Changes in volume of distribution
- Altered elimination via mechanical support devices (i.e. CRRT, ECMO)
CONCLUSIONS
- There is a lack of data to aid the clinician on the frequency, classes of agents to use and duration of antimicrobial therapy in sepsis patients
- A detailed consideration of all host, pathogen, source, clinical response and treatment related factors should be considered in determining the optimum course for sepsis patients.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.