Machine Learning Predictive Spesis Models
SUMMARY
- Various machine learning sepsis prediction models exist and are promoted to facilitate early identification of patients at high risk for sepsis.
- Most are based on electronic health record data.
- Results range from producing improvements in outcomes to poor discrimination and calibration with poor predictability of sepsis onset and no difference in outcomes.
REVIEW
- Early recognition and treatment of sepsis is key to driving successful outcomes.
- However, the heterogeneity in sepsis presentations makes early identification difficult.
- Interest in an automated sepsis prediction model has existed for years.
- These tools have produced variable results in the ability to predict sepsis and patient outcomes.
- In 2 different reports, the EPIC sepsis predicting model had poor discrimination and calibration in predicting onset of sepsis, but did improve antibiotic timing in a community hospital setting.
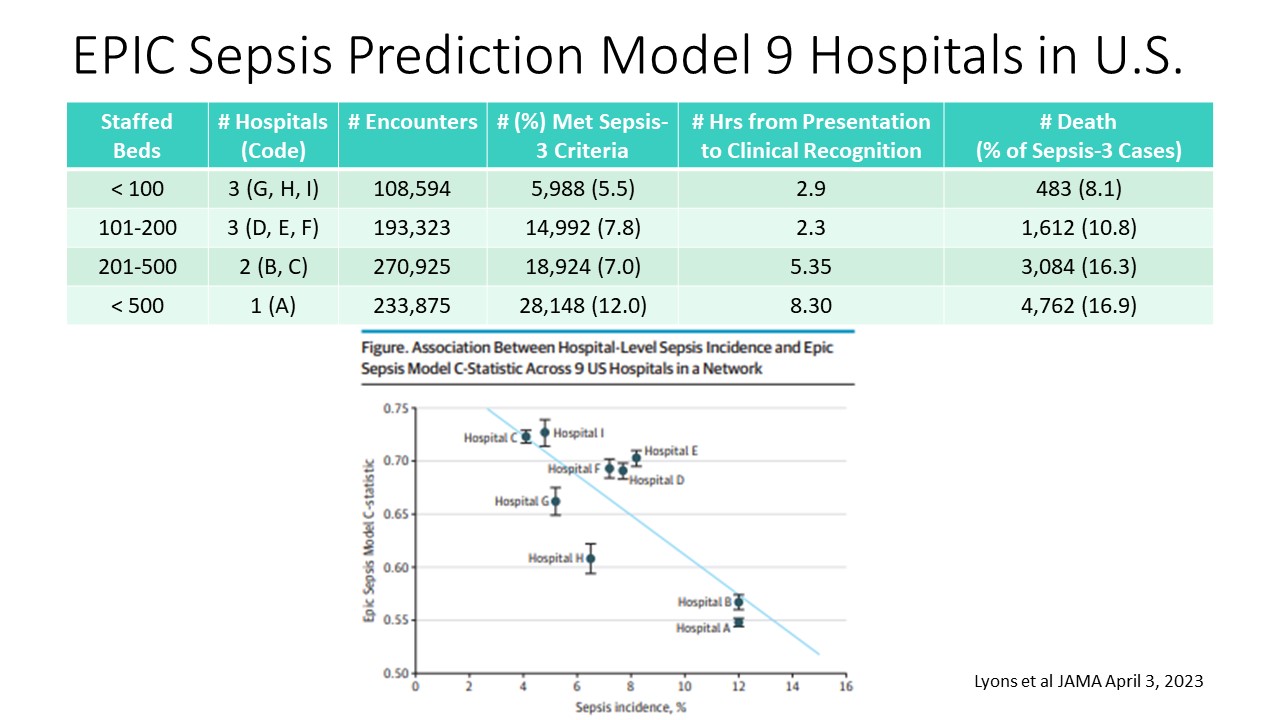
- In a recent research letter, data (Lyons et al JAMA April 3, 2023) from 9 hospitals with 806,696 patient encounters was reported.
- Sepsis-3 criteria was used from EHR data
- Sepsis onset was based on wither antibiotics being ordered or cultures
- Performance of the EPIC sepsis model was negatively correlated with the incidence of sepsis, comorbidities and cancer prevalence.
How These Findings Should Be Used for Machine Learning Predictive Sepsis Models
1. Using EHR Data is Challenging:
a. Heterogenous data within EHR’s make it difficult to create a single model for clinicians to use.
b. Sepsis is a clinical diagnosis
c. Mean hours from presentation to clinical diagnosis ranged from 2.3 to 8.3 above.
2. One Size Does Not Fit All
a. Customization of workflow within a setting is essential.
b. Development of these workflows should ask: How, When, Which threshold values to be used.
c. This requires close collaboration with staff and bedside clinicians
3. Improved Patient Stratification
a. Based on the November 2021 Surviving Sepsis Campaign Guidelines:
i. High Probability of sepsis patients should receive antibiotics within 1 hour
ii. Moderate probability of sepsis patients should receive antibiotics within 3 hours, after a thorough search for other etiologies
iii. Low probability of sepsis warrants assessment for non-infectious causes of systemic inflammation.
CONCLUSION
- Standardized sepsis predictive models should be characterized and trained at each site before widespread use.
- Integration into workflow is an important consideration.
- These tools are adjunctive and should not replace clinical judgment.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.