How Should We Screen for Sepsis?
How Should We Screen for Sepsis?
SUMMARY
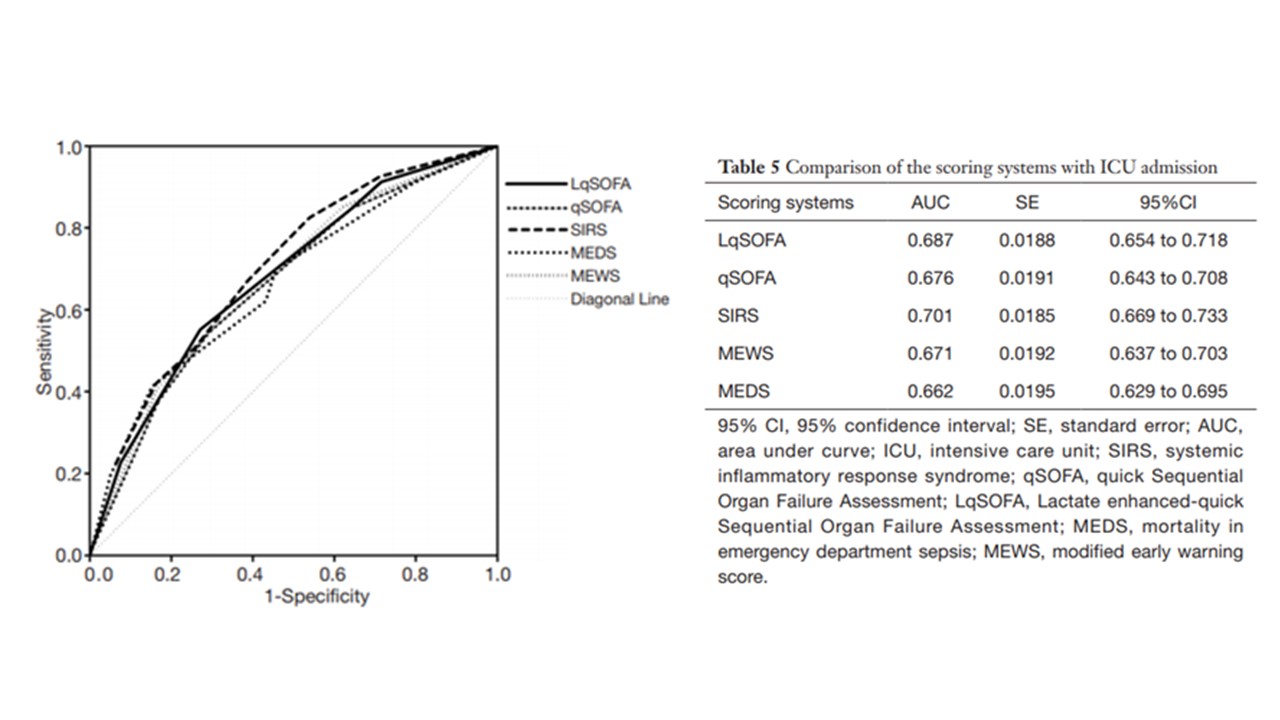
- Sepsis screening remains a major challenge, especially in varied settings.
- Effective screening impacts treatment, quality of care initiatives and outcomes.
- Different screening tools may be needed based on the clinical setting.
- The tool at each site may need to be tuned uniquely for that population and be validated for effectiveness and outcomes.
REVIEW
- Early and accurate assessments play an important role in the timely identification and management of sepsis. Delays in diagnosis or initiation of effective treatment has poorer outcomes and greater costs.
- Rapid and simple screening tools are the most desirable, especially in the Emergency Department (ED) to identify patients needing clinical care.
- Many screening tools involve laboratory parameters which may take time to provide results.
- This has led to the development of imperfect screening criteria using proxy markers.
- Deficiencies in current screening tools:
- Improvements in sensitivity, specificity, positive and negative predictive values, availability and performance are important.
i. Simple to remember tools (i.e. SIRS) do not account for organ dysfunction.
ii. Evidence demonstrating accuracy is limited.
iii. Dependent of absolute cut-points.
iv. Not tuned to local conditions.
v. Must balance excessive notifications with delays in assessments.
vi. Limited availability of data.
vii. Non-specific for sepsis.
Areas For Future Improvement
- Best screening tool for each setting has not been established.
- Sepsis screening needs to be aligned with work flow changes and outcomes.
- Screening should initially focus on suspected infection.
- Identification of a dysregulated host response to infection with clinical markers is lacking.
- Improved markers for identification and validation of acute organ dysfunction are needed.
CONCLUSIONS
- Improved categorization of patients needing sepsis assessment will aid in the delivery of improved clinical diagnosis and effective therapies.
- Warning systems may need to be specialized for the different settings (ED, ward, ICU).
- Each one must be tuned to optimize notification volume and effectiveness unique to the setting.
- Predictive analytics may be able to meet this challenge but must be validated in their ability to optimize performance and linked to improved outcomes.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.