Sepsis Now Part of CMS Value-Based Purchasing Program
SUMMARY
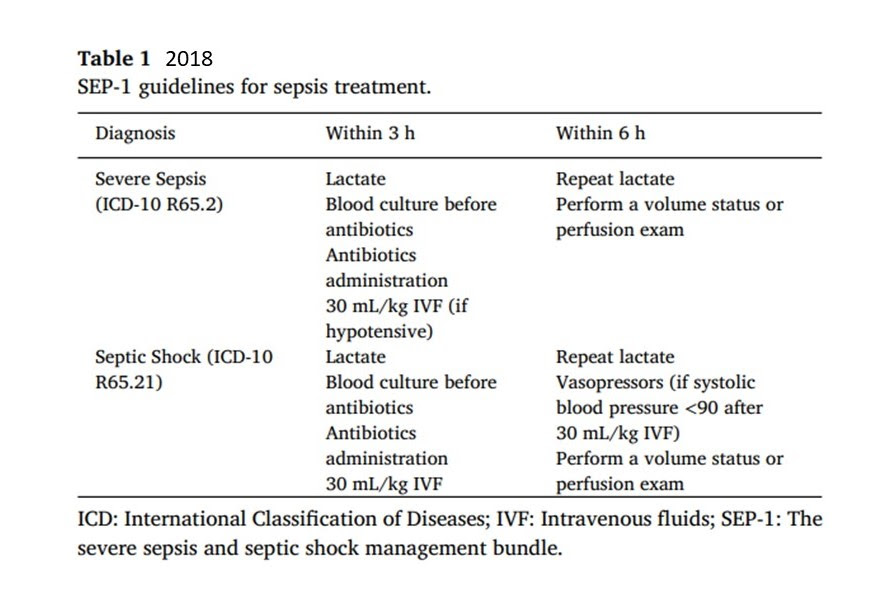
- The U.S. Center for Medicare and Medicaid Services (CMS) Severe Sepsis and Septic Shock Early Management Bundle (SEP-1) lays out the process for providers to follow in the care of the sepsis patient.
- First published in 2015, then amended in 2018, CMS is recommending SEP-1 become added to the Hospital Value Based Purchasing Program (HVBP) starting FY2026.
- Coupled with a multiplier for care of the underserved patient population, the SEP-1 measure can net a 2.8% increase as part of the inpatient prospective payment system.
- However. specific conditions must be met.
BACKGROUND
- The CMS SEP-1 sepsis measures became quality indicator metrics in 2015
- The goal of SEP-1 was to promote quality and cost effective care on a national level.
- 2018 unveiled the newest version of the sepsis guidelines and was very similar to the 2015 guidelines.
- Hospital sepsis compliance data became publicly available.
- The FY 2024 CMS Hospital Inpatient prospective payment system (PPS) made a number of rule changes.
- The only new measure was the addition of the Severe Sepsis an d Septic Shock Management Bundle.
REVIEW
- The global burden of sepsis is not in debate.
- The continued variability of care of sepsis still remains
- The value of compliance with the CMS SEP-1 sepsis bundles has yet to be resolved.
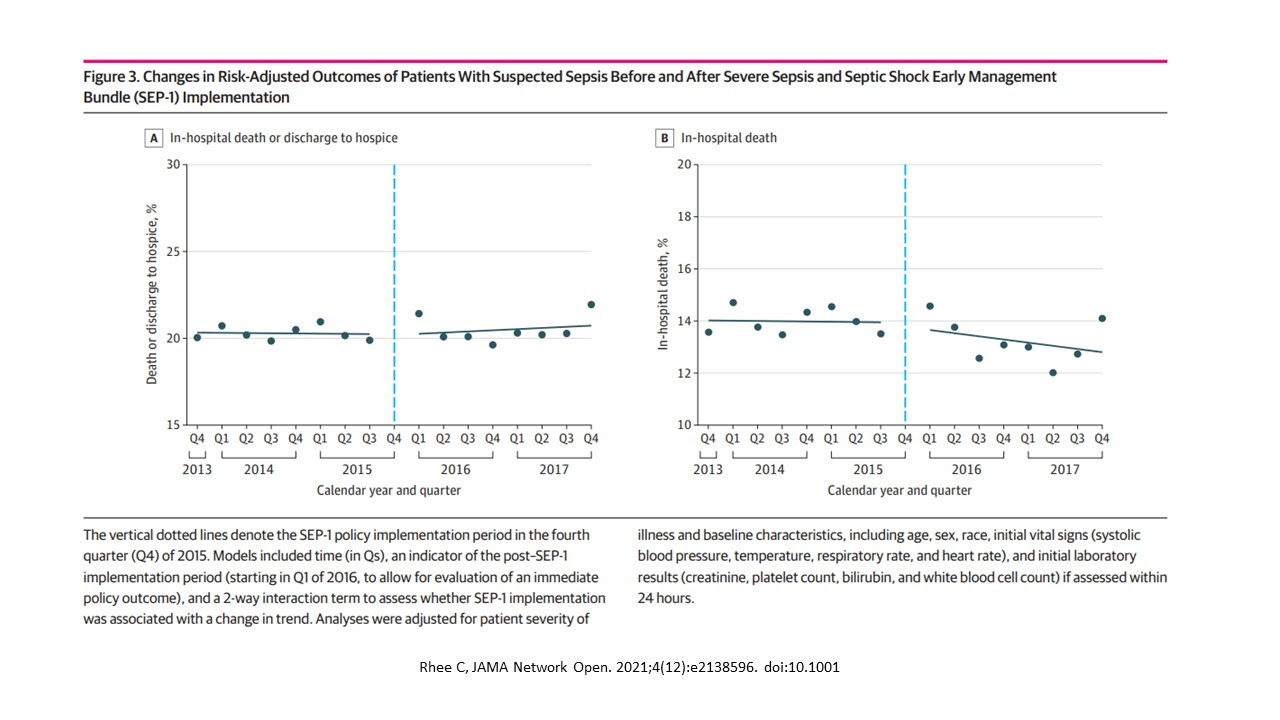
- Rhee et al JAMA Netw Open. 2021;4(12):e2138596. doi:10.1001
- No change in mortality after SEP-1 initiation
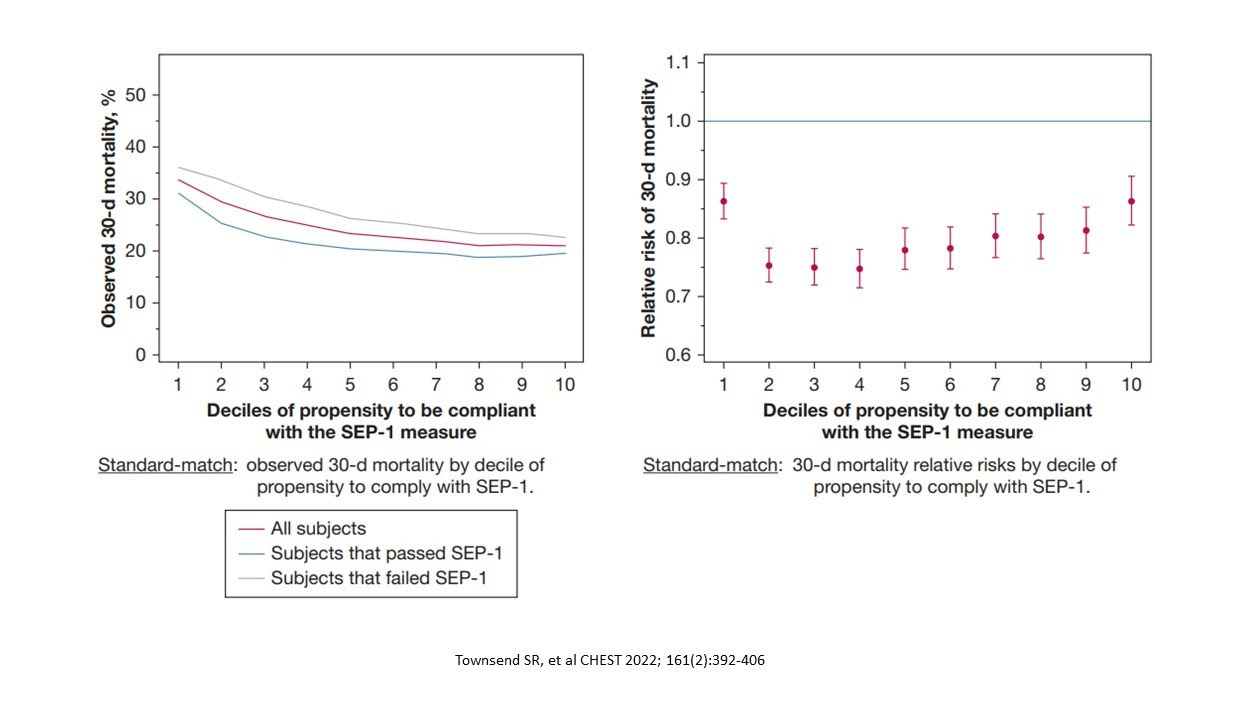
- Townsend SR et al CHEST 2022; 161(2):392-406
- Compliance with SEP-1 decreased 30 day mortality
- Potential reasons for varying results with SEP-1 compliance
- Changing guidelines and definitions
- 4 Surviving Sepsis campaign guidelines
- 3 International Consensus definitions
- SEP-1 uses outdated definitions (Sepsis-2 definitions from 2001, published in 2003).
APRIL 2023
- CMS issued fiscal year 2024 hospital inpatient prospective payment system (IPPS) rules
- An overall 2.8% increase for inpatient IPPS payments will occur
- Hospitals not submitting quality data will only get 2.05% increase
- Hospitals not meeting EHR meaningful use will only get 0.55% increase.
- Hospitals not meeting both will get a payment decrease of 0.2%
- Significant changes to Hospital Value Based Purchasing Program (HVBP)
- Beginning in FY2026 CMS will add a Health Equity Adjustment (HEA)
- HEA will be a total performance score consisting of 2 parts:
- High quality performance
- Extent to which underserved patients are served = proportion of dual eligible patients for Medicare and Medicaid
- Points will be assigned based on whether the hospital scores in the:
- Top Third
- Middle Third
- Bottom Third
- THE ONLY NEW MEASURE ADDED TO HVBP IS SEVERE SEPSIS AND SEPTIC SHOCK MANAGEMENT BUNDLES
CONCLUSIONS
- CMS Sepsis SEP-1 management bundle elements have evolved from:
- 2015 Quality Performance Items
- 2018 Publicly Available Quality Data
- FY2026 Tied to hospital reimbursement
- Although the net 2.8% increase is felt by many to be inadequate, the amount maybe lower if inpatient prospective payment programs are sub-optimal
- Health systems must be ready for this sepsis reimbursement change.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.