Centers for Disease Control and Prevention Sepsis Initiatives
SUMMARY
-
The U.S. Centers for Disease Control and Prevention (CDC) has proposed the “Adult Sepsis Event Toolkit” – 2018 (ASE Toolkit), and the “Hospital Sepsis Program Core Elements” – 2023 (Sepsis Program Core Elements).
-
The Program Elements were developed to help hospitals develop programs to monitor and optimize sepsis management and outcomes.
-
The goals of this ASE toolkit was to provide health systems a more objective measure to track sepsis incidence and outcomes based on the Sepsis-3 definitions.
REVIEW
CASE TOOLKIT (2018)
-
The CDC ASE Toolkit is for identifying sepsis in hospitalized patients.
- The ASE Toolkit removes SIRS criteria from the definition of sepsis.
-
SIRS criteria are common and nonspecific.
-
SIRS criteria risks both over-detection and under-detection of sepsis.
-
SIRS has also been excluded from the Sepsis-3 Consensus Conference definition of sepsis.
-
-
THE ASE Toolkit excludes the use of ICD-10 codes to identify patients with infection.
-
ICD-10 codes are often inaccurate in the identification of sepsis.
-
Reported sepsis cases increase when ties to ICD-10 codes with financial implications.
-
-
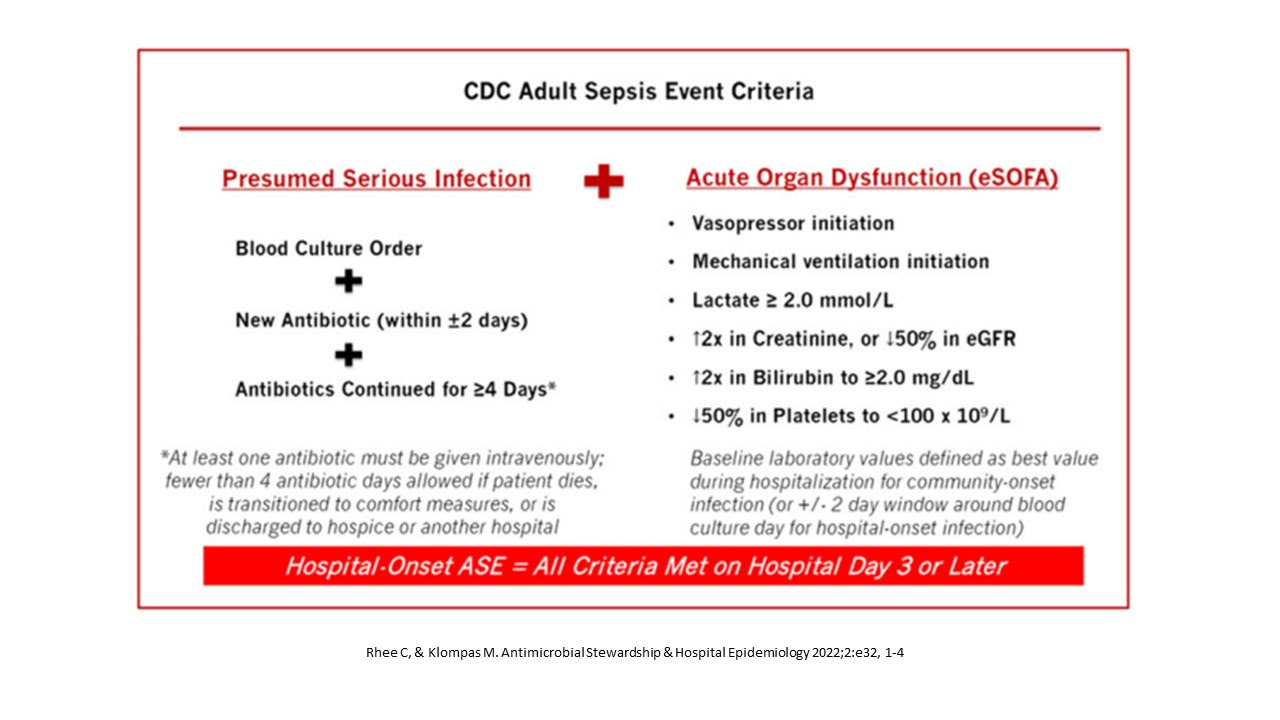
ASE defines suspected infection as:
-
A blood culture ordered (regardless of result) AND
-
Antibiotic administration:
-
Within 2 days of blood culture
-
A duration of at least 4 days
-
-
-
ASE Organ Dysfunction is present with:
-
Initiation of vasopressors
-
Initiation of mechanical ventilation
-
New changes in serum creatinine, total bilirubin or platelet count.
-
Organ dysfunction definition does not consider:
-
Mental status
-
Vasopressor dose
-
Urine output
-
Blood gas results and fraction of inspired oxygen
-
-
-
Limitations of ASE Toolkit:
-
Excludes patients without blood cultures
-
Excludes hypotensive patients not requiring vasopressors
-
Excludes patients receiving non-invasive respiratory support.
-
SEPSIS PROGRAM CORE ELEMENTS (2023
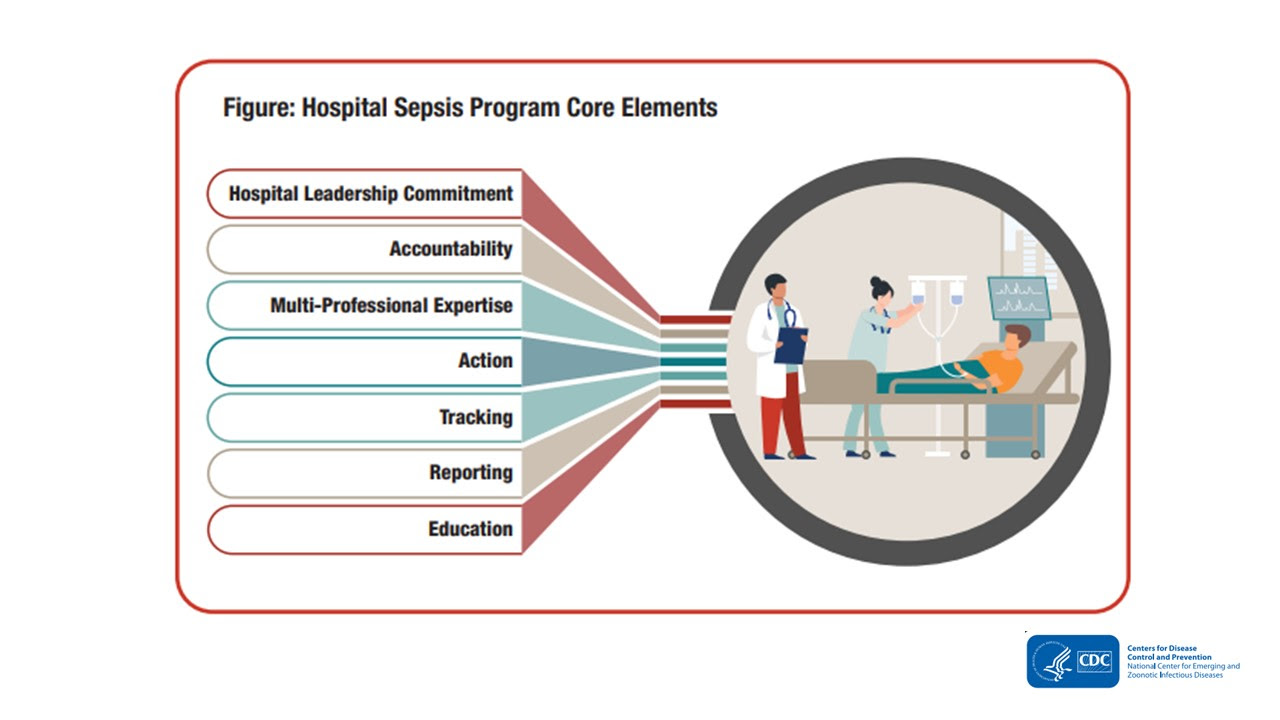
- Developed to assist hospitals in the development of multiprofessional programs designed to monitor and optimize the management and outcome of sepsis.
-
Complements existing sepsis guidelines and best practices.
-
Includes:
-
Evidence based clinical management
-
Education (clinicians, patients, families, caregivers)
-
Tracking and reporting treatment & outcomes.
-
-
Emphasizes hospital leadership
-
Addresses all hospital based sepsis activities (not just improving the patient selection process):
-
Education
-
Track sepsis management
-
Reporting of outcomes
-
-
Not just focused on the first 6 or 24 hours of sepsis management.
CONCLUSIONS
-
The Centers for Medicare and Medicaid have had a dramatic impact on focusing attention to sepsis with the Severe Sepsis/Septic Shock Management Bundle (SEP-1), which is now being implemented for a pay for performance measure.
-
Considerable controversy with SEP-1 has resulted in the CDC developing 2 documents over the past several years to implement an improved risk adjusted sepsis outcome measure and hospital guide for optimal program development.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.