Two Standards of Sepsis Care – The Nighttime Effect
SUMMARY
- Services in most hospitals differ between day & night or weekend shifts.
- With clinical staff and hospital resources typically diminished during “off hours”, there is increased risk of varying diagnosis, treatments and outcomes of various time sensitive conditions.
- Limited data indicates, sepsis is no exception to the “Nighttime Effect”.
REVIEW
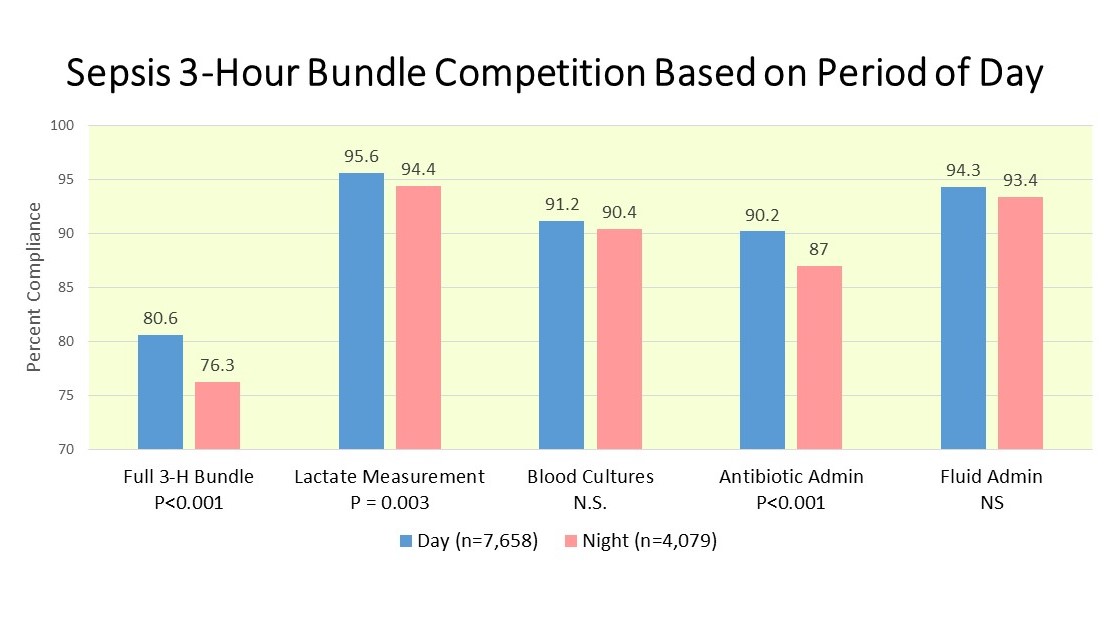
- The largest study on the Nighttime effect was recently published (Ranzani et al Ann Am Thorac Soc 2020;17:980-987).
- 10 private hospitals in Sao Paulo Brazil from 2010-2017
- 11,737 sepsis patients
- 8,733 severe sepsis/3,004 septic shock
- Adjusted for case mix
- Daytime: 0700 – 1859/Nighttime 1900 – 0659
- Weekends Friday 1900 to Monday 0659
RESULTS
- Patients treated during daytime hours had more frequent:
- Lactate Measurement
- Early antibiotic administration
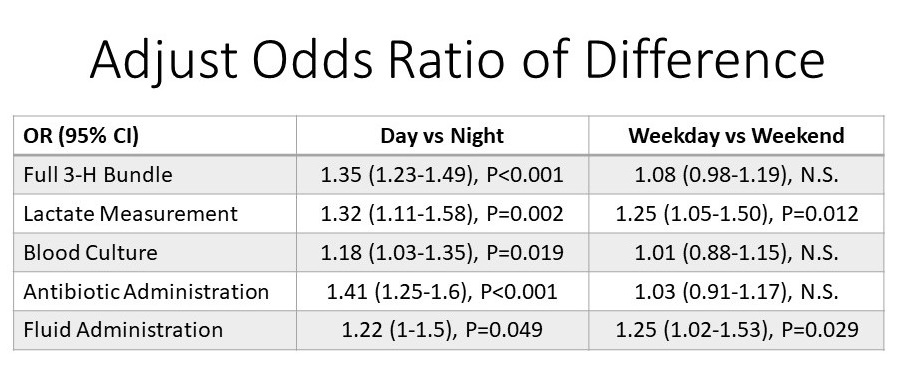
- The adjusted Odds Ratio showed a difference between Day vs Night outcomes but not weekday vs weekend outcomes.
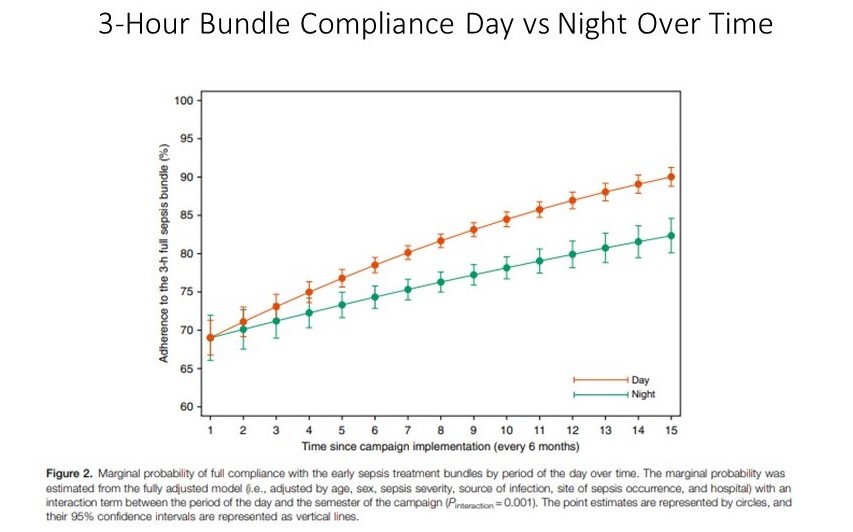
- The gap between day vs night patient 3-hour bundle completion widened over the study period.
- In comparison, a recent study (You et al Critical Care 2022;26:43) in 2,000 septic shock patients showed improved timely antibiotic administration during nighttime vs daytime, with a significantly lower staffing ratio at nighttime.
- They also had higher completion of the 3-hour bundle, although other individual components were not different between the groups.
CONCLUSIONS
- Early recognition and management of sepsis is key to improving outcomes.
- The impact of off hours admissions on various disease states is well studies in terms of diagnosis, treatment and clinical outcomes.
- Limited data in patients within the emergency department indicate they are also subject to “The Nighttime Effect” of limited resources and potentially less experienced staff.
- Septic shock patients may be the exception as this condition is more easily recognizable as compared to sepsis without shock.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.