Septic Shock: The Balance Between Fluid and
Vasopressor Administration on Mortality
SUMMARY
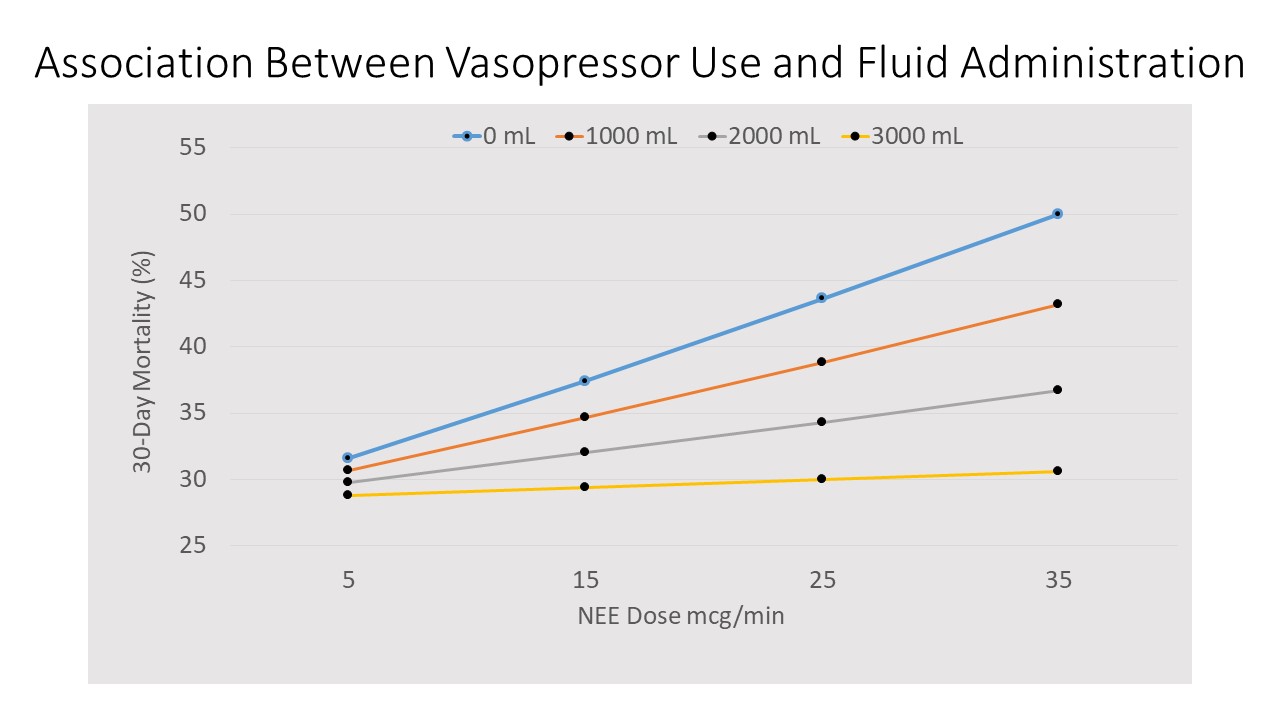
- Increasing doses of vasopressors within the first 6 hours are associated with increased mortality unless paired with at least 2,000 mL of fluid administration.
- Increasing vasopressor doses are associated with increasing mortality over the first 24 hours of septic shock.
- Additional evaluations optimal balance between fluid and vasopressor administration.
BACKGROUND
- Vasopressors are recommended to be initiated within 6 hours of sepsis in hemodynamically unstable patients after fluid resuscitation.
- The ideal balance between fluid and vasopressor administration in patients with septic shock is not known.
- Current guidelines outline WHAT to do (fluid resuscitation followed by vasopressors in hemodynamically unstable septic shock patients), but there is a lack of guidance on HOW to achieve this desired hemodynamic endpoint within the bundle.
- The association between administration of fluids and/or vasopressors to achieve the desired hemodynamic endpoint and impact on mortality is unknown.
REVIEW
A recent review of 616 patients with septic shock from 33 hospitals retrospectively evaluated vasopressor administration following fluid resuscitation.
- Data from September 1, 2017 – February 1, 2018, consecutive septic shock patients
- The goals were to:
o Determine if vasopressor response varies depending on fluid administration volume.
o Determine the association between vasopressor dosing and 30-day in-hospital mortality.
- Data from 12 hours before to 24 hours following shock onset.
- Fluid administration was the total volume of all fluids and blood products administered from 0-24 hours.
- Vasopressors:
o Dopamine; epinephrine; norepinephrine; phenylephrine; vasopressin
o All doses converted to “Norepinephrine Equivalents” (NEE).
o NEE determined for 0-6 hours and 0-24 hours with time-weighted rules.
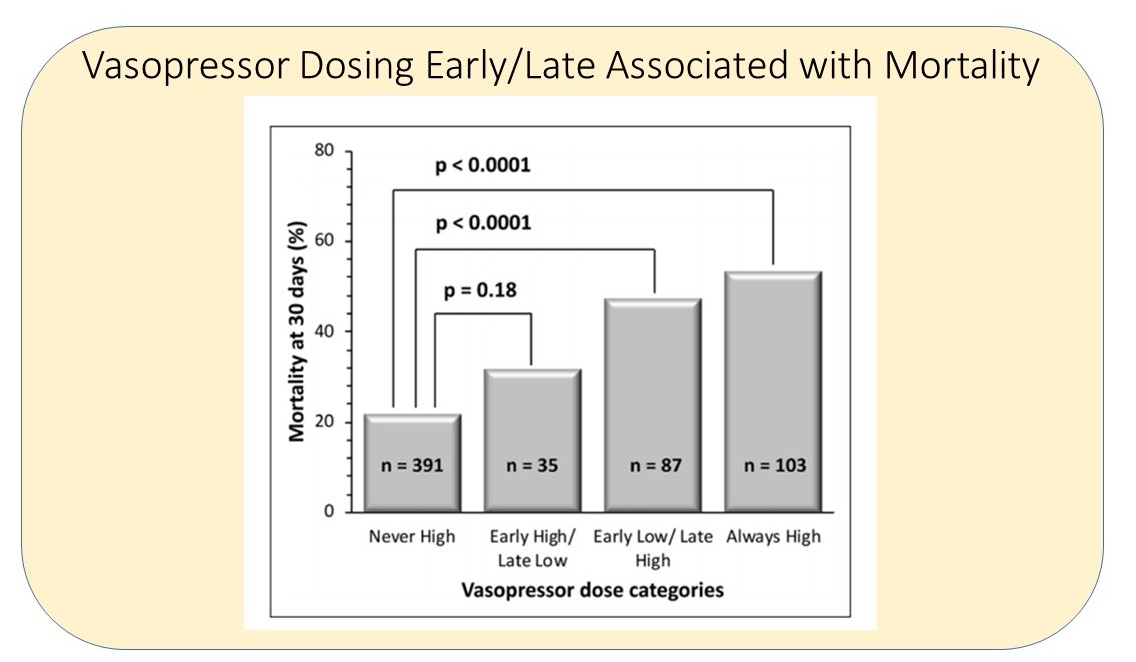
- Vasopressor Dosing Intensity (VDI) across the 2 time periods were categorized as:
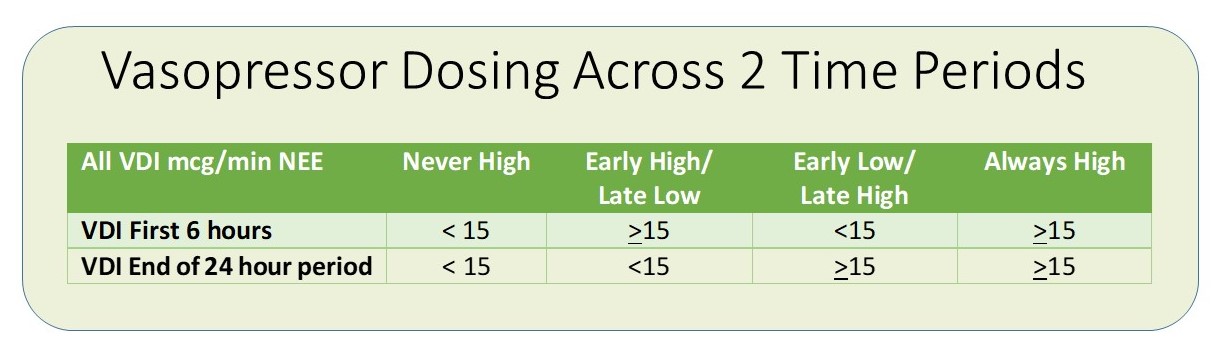
- 0-6 hour: Increased 30-Day mortality with increasing VDI with less than 2000 mL fluid administration
-
0-24 hour: Increased VDI also associated with increased 30-Day mortality, but did not vary with fluid administration
o Every 10 mcg/min increase in VDI increased odds of 30-Day mortality by 33%.
- Patients who were in the Early High/Late Low VDI dosing group were associated with lower mortality rates compared the Early Low/Late High VDI group.
-
Common Fluid and Vasopressor strategies to achieve desired mean arterial pressure (MAP).
o Start vasopressors at a moderate dose with gradual increase.
o Administer incremental fluid boluses while gradually increasing the vasopressor dose.
o Start higher dose of vasopressor and reduce the dose after MAP achieved.
o Restrictive fluid strategies early on, combined with earlier aggressive vasopressor support.
CONCLUSIONS
-
The optimal balance between fluid and vasopressor administration is unknown and needs to be evaluated.
- The minimum threshold of fluid administration prior to vasopressor initiation is unknown.
- Volume administration of less than 2000 ml combined with vasopressor administration was associated with higher trends in mortality.
- Individualized therapy balancing fluid and vasopressor dosing in terms of amount and timing are necessary.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.