Efforts to Improve Sepsis Outcomes Before Hospitalization
SUMMARY
- Most sepsis cases begin outside the hospital with a diverse range of clinical findings.
- Evaluation of sepsis patients should include administrative claims data coupled with physiologic and laboratory data.
- Characterization of sepsis prior to hospitalization can highlight key areas for education and preemptive care to improve identification, interventions and monitoring to improve progress of illness and outcomes.
REVIEW
Fay et al (2020) retrospectively reviewed the medical records, prehospital and discharge information of 1,078 adult patients from 29 hospitals discharged with sepsis or septic shock between October 1, 2014 and September 30, 2015.
Major Findings for Consideration
1. PATIENT CHARACTERISTICS
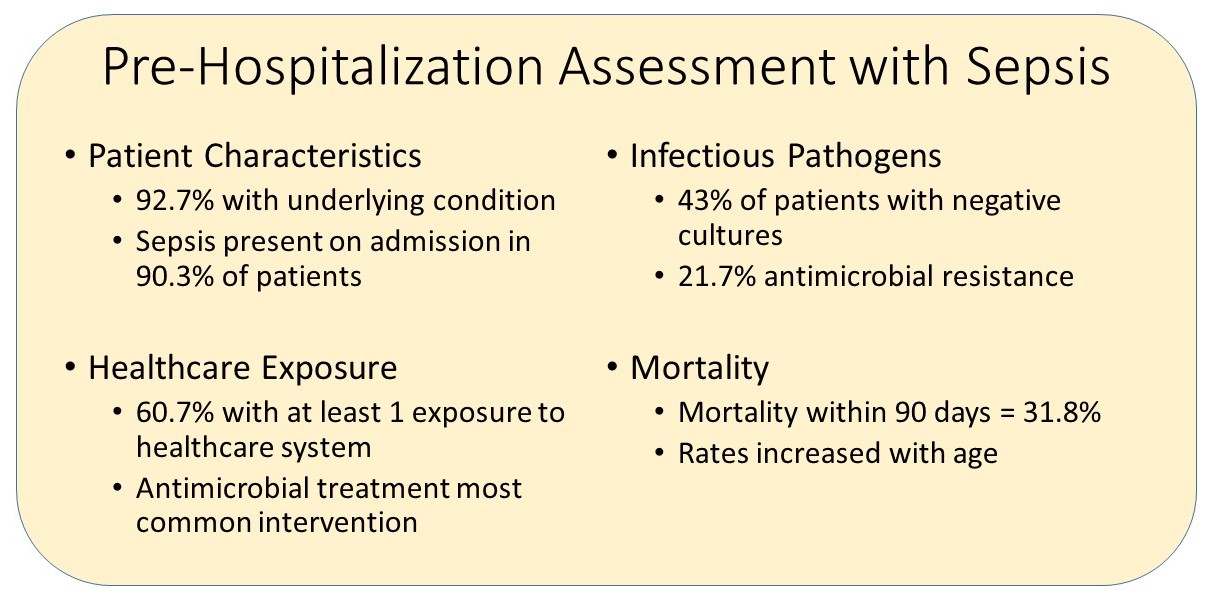
- 92.7% of patients had at least 1 underlying comorbidity condition
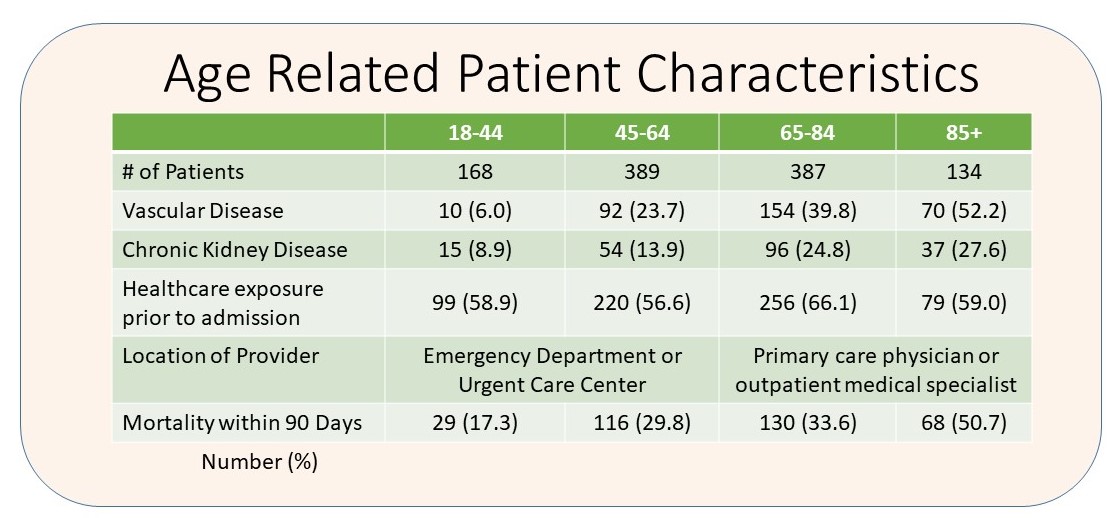
- The prevalence of vascular disease and chronic kidney disease increased with age
- Sepsis was present on admission in 973 (90.3%) of patients
- Most patients (806, 74.8%) were admitted from a private residence
2. HEALTHCARE EXPOSURE
- 654 patients (60.7%) had at least 1 exposure, which did not vary by age, to the health care system prior to admission
- Some form of medical treatment was provided to 41.5% of patients within 30 days of hospital admission
- The most common treatment was prescribing an antimicrobial agent (30.4%)
- Older patients, 65 years and older, typically visited a primary care physician or outpatient medical specialist
- Younger patients, less than 65 years, primarily used an emergency department or urgent care center
3. INFECTIOUS PATHOGENS
- Bacterial cultures were obtained in 1,069 patients (99.2%)
- Sepsis associated pathogens were identified in 613 (56.9%) of patients
- 43% of patients had negative cultures
- When available, antimicrobial susceptibility testing demonstrated 21.7% resistance
4. MORTALITY FACTORS
- Total mortality:
- Within 5 Days: 13.2%
- Within 30 Days: 26.4%
- Within 90 Days: 31.8%
- Mortality within 90 days increased with increasing age
CONCLUSIONS
-
Most patients with sepsis have a pre-hospital exposure to health care which offers an opportunity to alter their disease course.
- Sepsis education to practitioners outside the hospital is an important opportunity
- Risk factors associated with death include:
- Increased age
- Presence of organ dysfunction
- Underlying condition
- 43% of patients do not have an identified sepsis associated pathogen
Fry K, Saplano MRP, Gokhale R, et al. Assessment of health care exposures and outcomes in adult patients with sepsis and septic shock. JAMA Network Open 2020;3(7):e206004
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





