Will Improving CMS SEP-1 Metrics Correlate
with Sepsis Clinical Outcomes?
SUMMARY
- CMS SEP-1 quality metrics can consume large amounts of hospital resources in order to collect and report their adherence.
- Hospitals solely focusing on the SEP-1 reporting should not assume this will automatically correlate with improved clinical outcomes of sepsis patients.
-
A solid sepsis program will ensure accurate SEP-1 data is reported but also drive process change on how to improve clinical outcomes.
BACKGROUND
- There remain many controversial areas of sepsis care, this includes the lack of a gold standard definition of sepsis as well as Time-Zero (T-0).
- The Centers for Medicare and Medicaid Services (CMS) began the sepsis quality metrics program (SEP-1) in 2015.
- Although not currently tied to reimbursement for sepsis patients, SEP-1 maybe moving in that direction. In 2018, CMS added the SEP-1 metrics to the Hospital Compare Program.
- SEP-1 data indicates wide variability in compliance with inconsistent improved outcome results.
REVIEW
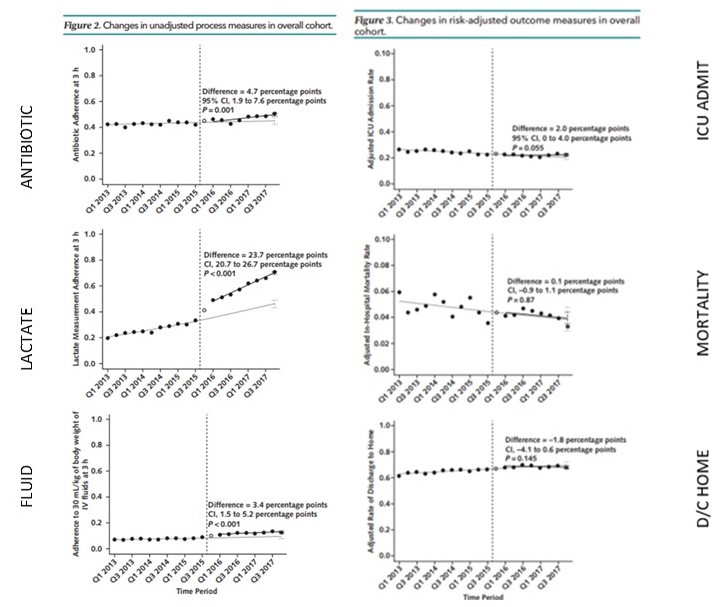
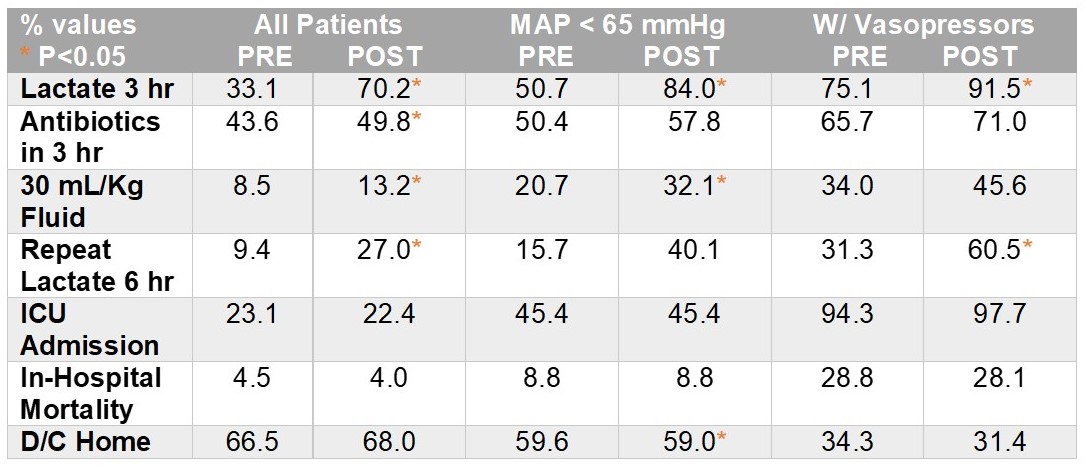
A recent retrospective review from the University of Pittsburgh Medical Center (UPMC) reviewed data form January 2013 through December 2017.
The goal was to determine what association, if any, existed between the implementation of the CMS SEP-1 quality metrics and sepsis treatments and outcomes.
Analysis from 11 hospitals in:
- 54,225 ED patient encounters with community onset sepsis only
- 29,051 patients PRE-SEP-1 Initiation
- 22,759 patients POST SEP-1 initiation
- 2,415 patients were excluded during the first quarter of SEP-1 initiation as a “washout period” (October 2015 – December 2015).
The UPMC assessment model calculated and compared an “expected” value for each outcome to the actual value in order to account for inherent changes in hospitals over time.
PRE & POST SEP-1 findings were:
- A significant improvement in lactate measurement, antibiotic administration and fluid administration occurred.
-
- The largest improvement was in lactate measurements
- There was a lack in any significant or clinically meaningful improvement in clinical outcomes in the total population or subgroups.
CONCLUSIONS
- The patients in this study did not appear to have a high level of illness severity.
- In 2017, UPMC SEP-1 compliance was only 38%, indicating low adherence after 2 years of CMS reporting
- The CMS SEP-1 measures are more about processes of care rather than outcomes and how to improve care
- Focusing on improving CMS SEP-1 measures does not automatically improve clinical outcomes.
- A quality sepsis program will include accurate SEP-1 reporting as well as process changes to improve clinical outcomes.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





