Incidence of Sepsis in Hospitalized Patients
Summary
- Sepsis positive patients account for approximately 5 – 10% of hospitalized patients
- Location of sepsis patients within the hospital varies based on severity of the sepsis disease state, with approximately 50% of patients are admitted to the ICU
- The majority of patients have sepsis present on admission
- Cost and outcomes show a large disparity between patients with sepsis present on admission versus not present on admission
Background
Sepsis identification and management continues to be major challenges for healthcare systems throughout the world. Recent data indicates increased incidence of sepsis by 8.7% per year.
The global burden of sepsis has been estimated at 49 million cases and 11 million deaths (double previous estimates). Sepsis deaths now exceed the number of deaths from cancer which is estimated at 9.6 million people per year.
Hospital resources are disproportionally higher in sepsis patients. The average length of stay (LOS) is 75% greater than most conditions. The cost of sepsis in U.S. hospitals are the highest among admissions for all disease states. Recent medical data indicates costs from 2012-2018 have increased from previous estimates of $27 billion to $41.5 billion.
Review
Accurate estimates of sepsis are important to monitor interventions, allocations of resources and clinical treatment interventions. Most estimates rely on various methods to identify sepsis patients, the most common being clinical diagnostic codes or billing codes. Patterns of sepsis vary substantially geographically. In addition, the incidence of sepsis among patients with suspected infection is unknown.
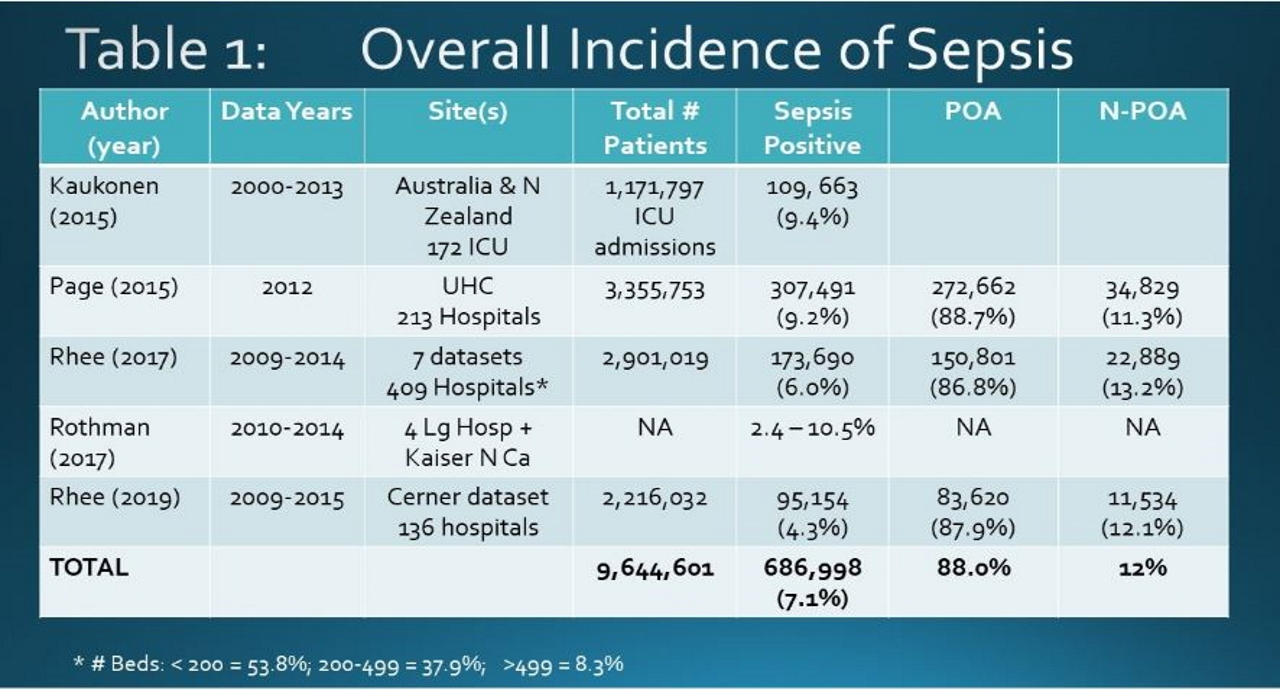
Table 1 reviews over 9.6 million hospitalized patients from large studies from various databases. The overall incidence of sepsis ranges from 2.4 to 10.5% with an average of 7.1%. Where available, the data indicates 88% of the cases are present on admission (POA) with 12% of cases not present on admission (NPOA). NPOA patients could include patients who presented with sepsis but were missed as well as those who developed sepsis as a complication after admission.
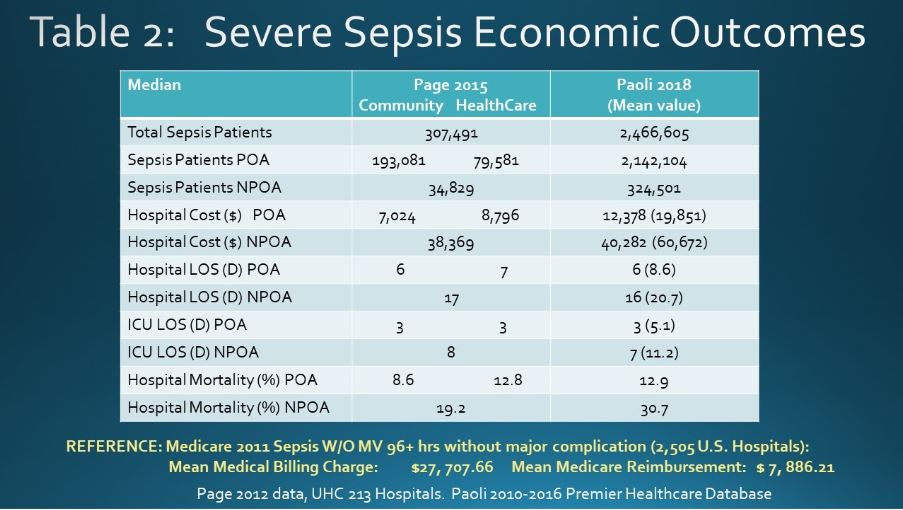
Table 2 reviews 2 large studies characterizing the different outcomes and costs between POA sepsis and NPOA sepsis patients. NPOA patients demonstrate higher ICU and hospital LOS, higher mortality rates. The hospital costs for a NPOA sepsis cases is several fold higher than POA sepsis cases.
Conclusions
- Of hospitalized patients, approximately 5-10% of patients will have a sepsis diagnosis.
- The majority of the sepsis cases are POA, typically through the emergency department
- There are dramatic differences in clinical outcomes and costs between POA and NPOA sepsis patients.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.