Largest Study of Sepsis Cases among Medicare Beneficiaries
It has been well established that the cost of sepsis care and its public health impact is tremendous. However, the current largest sepsis study based on recent Medicare data indicates it to be significantly higher than previous estimates.
Current Understanding
Currently quoted estimated cost of acute inpatient sepsis care is $23.7 billion, however, this data is from 2013 and published in 2016. Medicare patients as a subset comprised 61.5% of the total patients in this study. Therefore, total inpatient sepsis costs for Medicare beneficiaries would estimate downward to $15 billion.
The majority of inpatients with sepsis arrive to the hospital with sepsis present on admission (POA) and as their admitting diagnosis. Only a minority of inpatients have sepsis not present on admission (NPOA) due to either a missed diagnosis or as a post-admission complication. NPOA patients have poorer outcomes (longer length of stay, higher mortality) as well as a higher cost of care.
Largest Study To Date
A recent study by Buchman et al included more than 9.5 million inpatient Medicare sepsis hospital admissions spanning 7 years (2012-2018). They evaluated the incidence of sepsis as well as sepsis-associated mortality during the inpatient stay and up to 3 years after discharge. Payments made by Medicare evaluated hospital input and subsequent skilled nursing facility (SNF) costs. Additional considerations included:
- Changes from ICD 9 to ICD 10 over the study period
- Sepsis DRG codes
- Inpatient Medicare part A & B
- Medicare Advantage Plans
- Sepsis POA and NPOA
- 4 sepsis tiers: septic shock; severe sepsis without shock; non-severe sepsis origin; non-severe sepsis unspecified.
Results
- The number of Medicare beneficiaries with sepsis diagnosis increased steadily over the study period.
- The increase in sepsis cases was disproportionate to Medicare enrollment over the same time frame (22% increased enrollment; 40% increased sepsis rate) and not due to aggressive coding behavior.
- Although the actual numbers increase, the proportion of patients with the different tiers of sepsis remained relatively stable over time.
- Sepsis continued to be associated with increased risk of mortality up to 3 years after admission, with all-cause mortality of initial sepsis survivors being 60% at 3 years compared to 40% for non-sepsis inpatient admissions.
- Sepsis POA kept steadily increasing, whereas NPOA decreased.
- Mortality at 6 months: NPOA = 60%; POA = 40%
- Costs were more than double of NPOA vs POA pts.
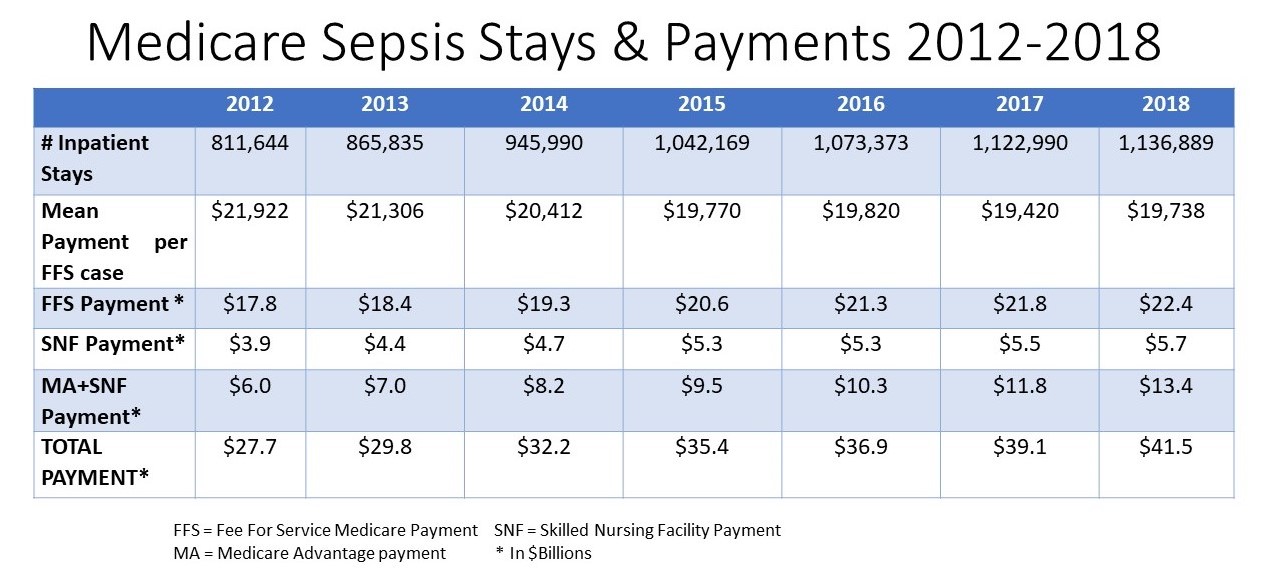
TABLE: Medicare Sepsis Stays & Payments 2012-2018
CONCLUSIONS
- The Medicare system saw a 40% increase in hospitalized sepsis cases with an estimated cost of over $41.5 billion.
- Although payment per case decreased, the increase in number of patients led to an overall increase in spending from $27.7 billion to $41.5 billion
- Actual national expenditure for sepsis greatly exceeds previously cited estimates.The majority of inpatients with sepsis arrive to the hospital with sepsis present on admission (POA) and as their admitting diagnosis. Only a minority of inpatients have sepsis not present on admission (NPOA) due to either a missed diagnosis or as a post-admission complication. NPOA patients have poorer outcomes (longer length of stay, higher mortality) as well as a higher cost of care.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.