Sepsis From a Financial Viewpoint
Sepsis has both a human suffering as well as a financial burden. In 2013, sepsis was the most expensive hospital condition and accounted for only 3.6% of hospital stays, but consumed a disproportionate 13% of total hospital costs amounting to $24 Billion.
In addition to clinical outcomes, economic evaluations assist in decision making of providing healthcare services. Critical care — and specifically sepsis — is an inherently complex care delivery arena, yet there is a paucity of cost evaluations.
Evaluating the Cost of Sepsis Care
The limited studies available demonstrate wide variability in cost evaluations.
Factors contributing to these variances include:
- Hospital vs ICU costs
- Differentiation between sepsis; severe sepsis; or septic shock (most of the data was published prior to the 2016 new definitions of Sepsis-3 and therefore are based on these 3 sepsis levels).
- Sepsis present on admission versus sepsis onset after admission
- Ability to adequately differentiate between costs and charges
In 2016, the Healthcare Cost & Utilization Project (HCUP) through the Agency for Healthcare Research & Quality (AHRQ) reported 2013 data, demonstrating that hospital length of stay (LOS) increased with sepsis severity (Table 1).
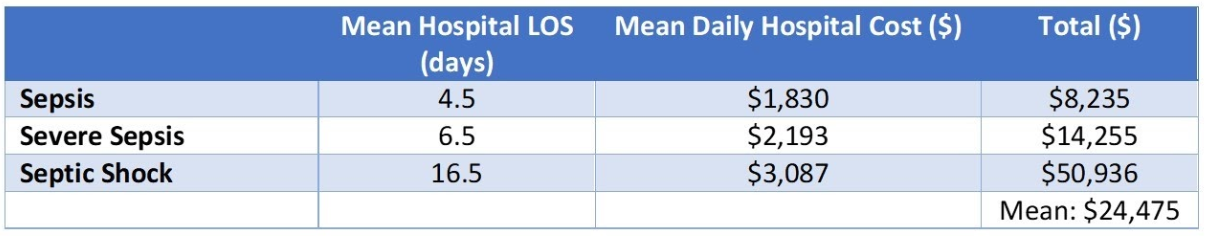
TABLE 1: Hospital mean LOS and daily hospital costs for sepsis conditions (HCUP 2016)
More recent reports from 2017 and 2018 report similar mean hospital patient costs for all sepsis patients ranging from $21,568 to $32,421.
A Closer Look
The cost of sepsis care gets more granular as we stratify the patient population.
Data examining sepsis diagnosis present on admission (POA), versus a diagnosis not present on admission (non-POA) is one such assessment. Sepsis non-POA, could indicate sepsis was acquired after admission, potentially as a complication, or that sepsis was missed on initial assessment.
Based on evaluation of a large healthcare database from January 2010 through September 2016 with over 2.5 million sepsis cases, every clinical metric and cost of care was consistently worse in the non-POA sepsis patient compared to the POA sepsis patient (Table 2).
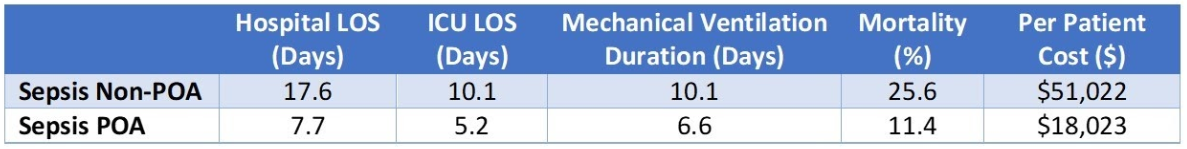
TABLE 2: Outcome Comparison of Sepsis Present on Admission vs Not Present on Admission
The severity of sepsis was also a stratifying discriminator (Table 3).
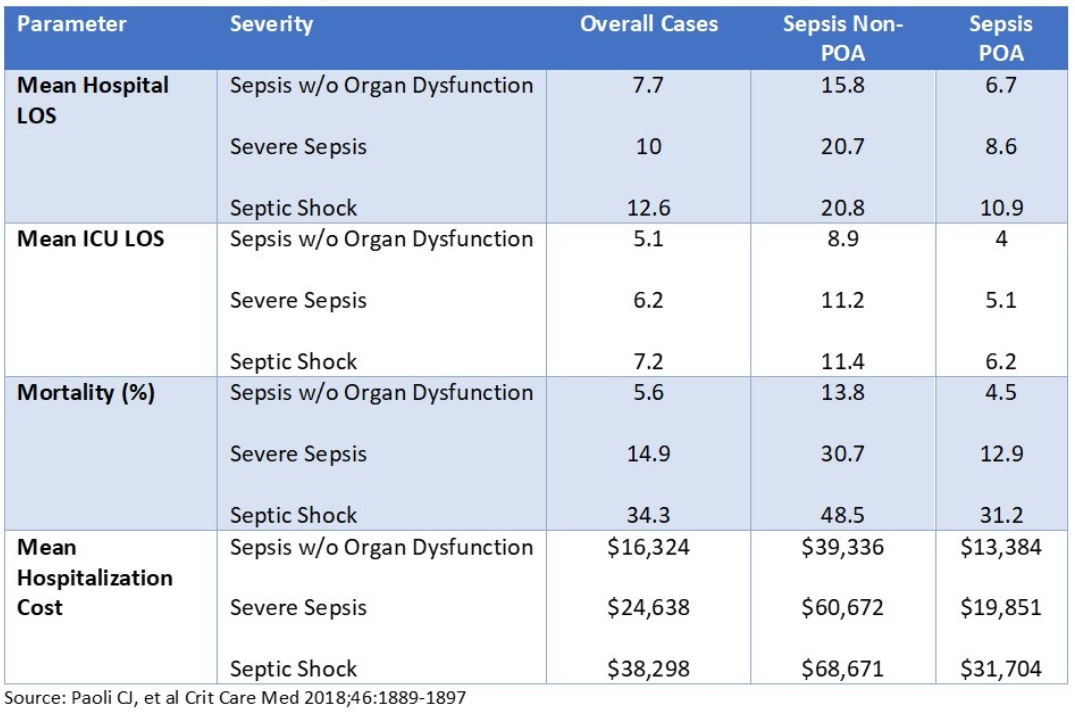
TABLE 3: Outcome Comparison of Sepsis Severity and Time of Diagnosis
Optimization = Cost Savings?
Sepsis screening and bundle compliance should result in optimizing the sepsis care process with earlier identification, improved survival and prevention of the more severe clinical manifestations of sepsis (i.e. severe sepsis and septic shock).
The aggressive monitoring and interventions should improve clinical outcomes but also have a beneficial effect on direct hospital costs, resulting in a financial savings.
However, there is also concern that reduced mortality may be accompanied with the consumption of additional costly ICU resources resulting in an increased cost of care.
An evaluation in 120 patients before and after implementation of a sepsis protocol indicated a cost savings (2007 dollars) of approximately $6,000 per patient (Table 4). This was predominantly due to a decrease in hospital LOS by 5 days (median) and a decrease in ICU (35%) and floor (30%) bed costs (P<0.03).
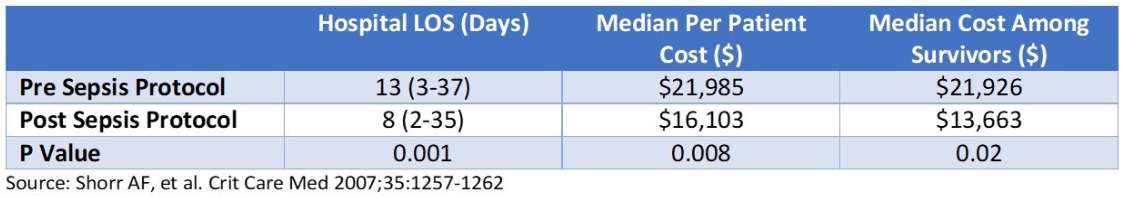
TABLE 4: Pre/Post Sepsis Protocol Cost Impact
Quality adjusted life years (QALY) provides an economic evaluation of an intervention. For sepsis, a recent study by Higgins et al and Wilcox et al determined a favorable lower cost with greater effectiveness for a number of the sepsis bundle elements. Unfortunately, many of the bundle elements remain without economic evaluations. Key to point out is the favorable cost effectiveness of a multi-disciplinary, coordinated quality improvement sepsis program to improve bundle compliance as well as ICU admission for the management of sepsis and septic shock.
Wilcox ME, et al Crit Care Med 2019:47:1011-1017
Higgins AM, et al J Intensive Care 2020; https://doi.org/10.1186/s40560-019-0412-2
Conclusion
Given the high burden sepsis places on individuals and the care delivery system, a high quality understanding of disease interventions and outcome are needed to better understand the most cost effective clinical interventions. The current literature provides little insight with considerable heterogeneity on financial sepsis results.
However, we can conclude:
- The best sepsis outcomes and cost considerations are when sepsis is identified early and with effective treatment.
- Sepsis which progresses to its severest form or identified after admission (due to either a missed identification or complication) has the lowest clinical effectiveness with the highest costs.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.