3 Key Factors for an Effective
Sepsis Performance Improvement Program
Sepsis Performance Improvement Program
SUMMARY
- There are several components to an effective sepsis performance improvement program.
- Having a sepsis performance improvement program in itself maybe more important than the specific content, there are a few mandatory components required for effectiveness.
- Including a large multidisciplinary clinical group is also essential for success.
REVIEW
- If you are convinced the Surviving Sepsis Campaign (SSC) Guidelines are worth pursuing, a Sepsis Performance Improvement Programs (SPIP) can aid with improved sepsis protocol adherence.
- Components of a SPIP are:
- Use of screening tools
- Multidisciplinary workgroup
- Involvement of Emergency Department, Ward and ICU
- Workflow changes in sepsis care pathways (independent of patient location)
- Metrics of success with frequency of measurements
- Data Collection forms
- Educational Process
- The exact sepsis bundle components resulting in the greatest reduction of mortality remains unknown.
- Therefore, it appears having a SPIP in itself may be more important than the specific content of the program.
3 KEY FACTORS TO SEPSIS IMPROVEMENT PROGRAM SUCCESS:
Factor 1: Sepsis Screening Tool
- Notification via an automated tool of a suspected infection or sepsis is a basic requirement.
- However, a screening tool is NOT THE SAME as a sepsis diagnosis.
- Sepsis diagnosis remains a clinical assessment
- The tool simply indicates which patients need a more in depth review.
- There are a large number of sepsis screening tools advocated for use.
- These consist of:
- SIRS Criteria
- Modified Early Warning Score (MEWS)
- National Early Warning Score (NEWS)
- Quick Sequential Organ Failure Score (qSOFA)
- The accuracy of these scores are highly variable, with none of them superior to the others in identifying sepsis across studies.
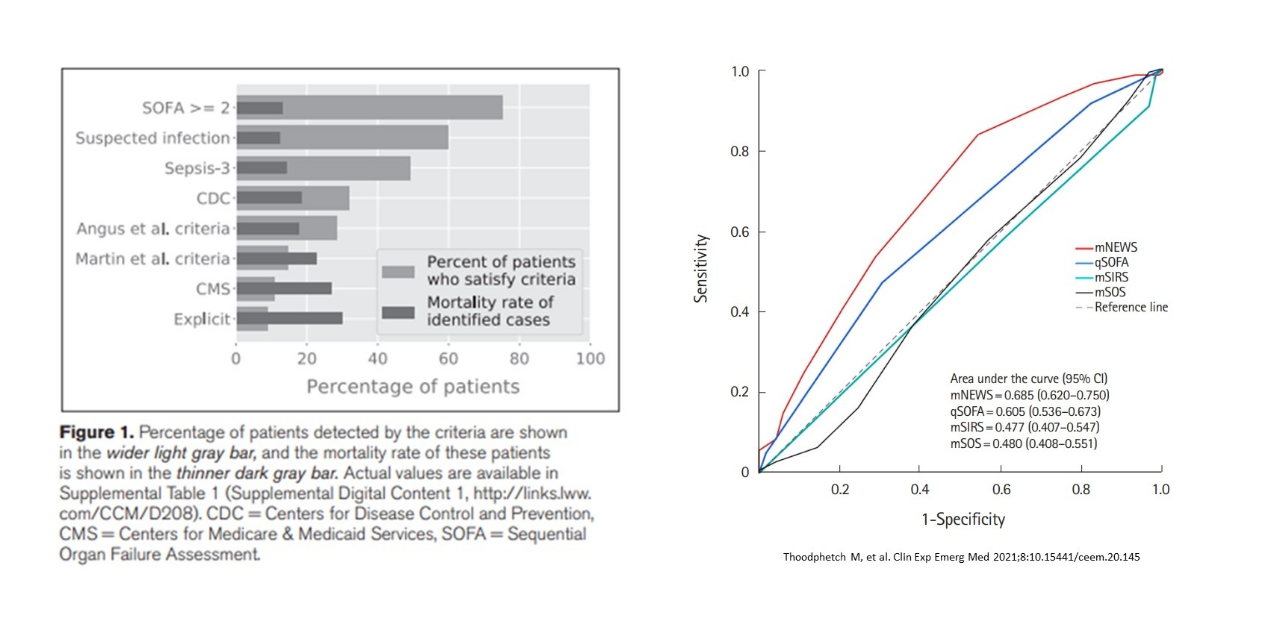
- All tools are subject to a large number of false positives, without a robust sensitivity, specificity or both.
- Due to its poor sensitivity, qSOFA has been recommended NOT to be used for screening purposes.
- To be most effective, all sepsis screening alerts should be combined with a mandatory and immediate clinical evaluation.
Factor 2: Sepsis Care Pathways
- Following the identification of a potential sepsis patient, the clinical pathways should be promptly initiated.
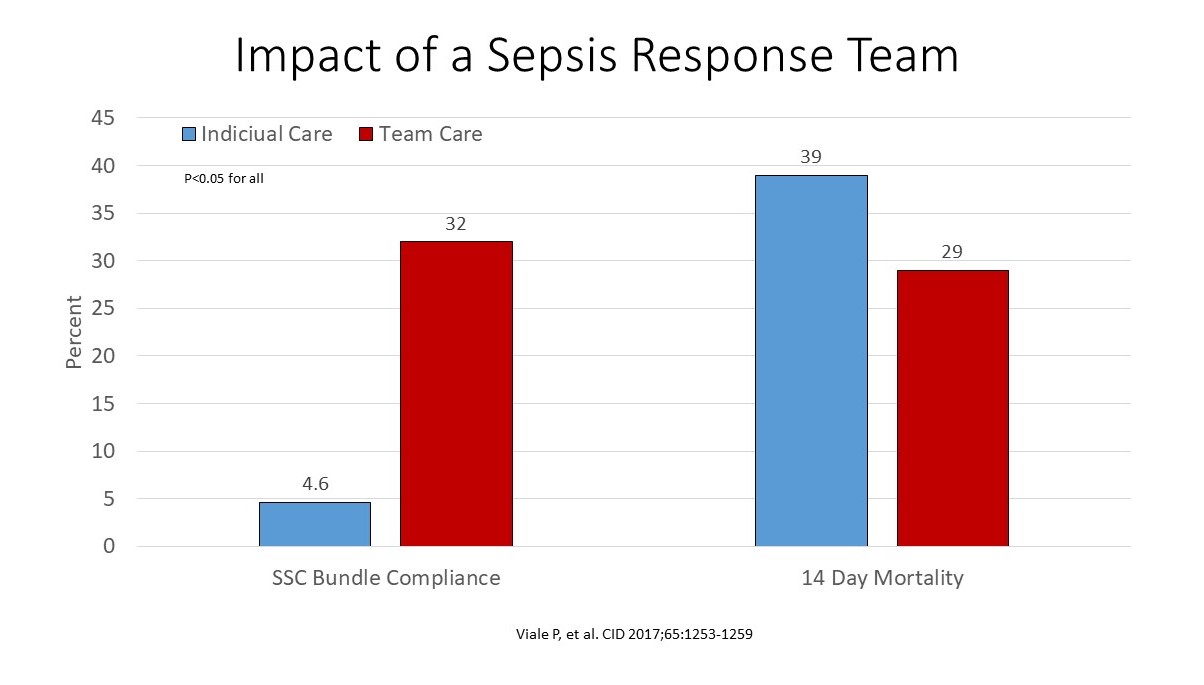
- The most studied critical process is the implementation of a sepsis response team as opposed to one consultant clinician.
- Dedicated teams which respond collectively contribute to improve bundle compliance and mortality
- Nurse-driven sepsis protocols are also a practical and beneficial collective team approach.
Factor 3: Sepsis Educational Program
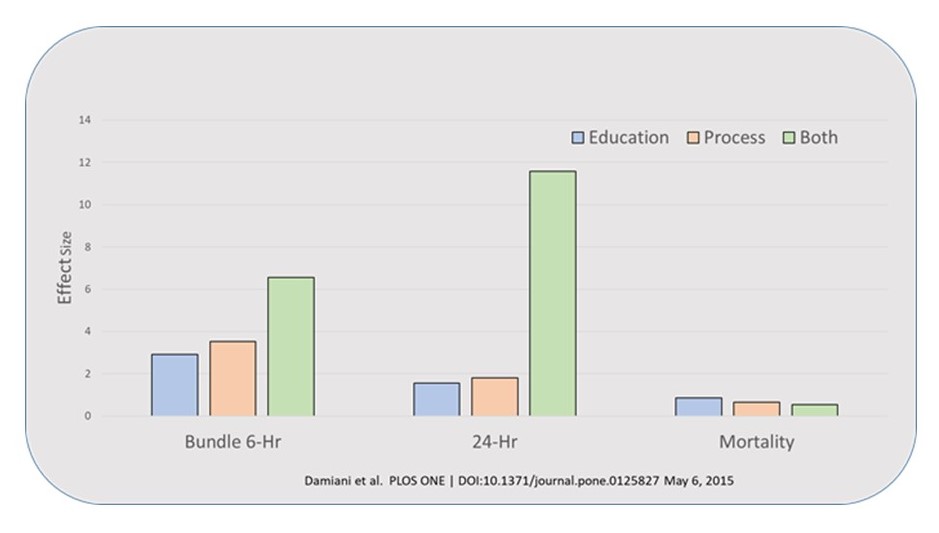
- Education is an essential piece of a SPIP to help raise awareness.
- This includes:
- Educational materials
- Lectures
- Bedside teaching
- Case examples
- Simulations
- Although educational programs alone can improve sepsis outcomes, the combination of education and process change.
CONCLUSIONS
- Regardless of the amount spent, treatment of sepsis is consistently expensive globally.
- Intensity of care of individual patients does not reflect the cost of healthcare sepsis expenditures
- General ward costs are greater than ICU costs, most likely due the length of stay being longer on the ward than ICU and a large proportion of patients admitted to the general ward.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.