Sepsis Associated Acute Kidney Injury:
Knowns and Unknowns
Knowns and Unknowns
SUMMARY
- By the time patients seek attention, most have already developed acute kidney injury.
- Sepsis associated acute kidney injury is a distinct syndrome different from other non-sepsis acute kidney injuries.
- There is a lack of specific interventions for the prevention and treatment of sepsis associated acute kidney injury.
- Once developed, sepsis associated kidney injury increases the risk of developing chronic conditions and is associated with higher mortality.
BACKGROUND
- Sepsis associated Acute Kidney Injury (S-AKI) is a distinct syndrome from other forms of AKI and occurs with the presence of sepsis without any other significant contributing factor(s) to the development of AKI.
a. Sepsis is the most common contributing factor for the development of AKI (40-50% of patients with sepsis in the ICU develop AKI as compared to an overall AKI rate of 5-34%).
b. AKI from any origin is associated with a higher risk of developing sepsis (40% of patients with AKI go onto develop sepsis).
- Sepsis and AKI make the patient vulnerable to each other.
- Little is known about the pathophysiologic mechanism or epidemiology of S-AKI a. Although AKI is typically associated with hypoperfusion and renal ischemic injury, these alone may not be the only mechanisms involved in S-AKI.
b. S-AKI can develop without renal hypoperfusion, clinical signs of hemodynamic instability and normal renal blood flow.
- Sepsis induced injury to any organ (including the kidney) contributes additional insults of:
a. Inflammation: The dysregulated immune response of sepsis contributes to renal tubular epithelial cell injury.
b. Microcirculatory Dysfunction: Multiple mechanisms contribute to microcirculatory changes causing organ dysfunction without hemodynamic instability.
c. Metabolic Reprogramming: Cell survival is prioritized at the expense of organ function.
REVIEW
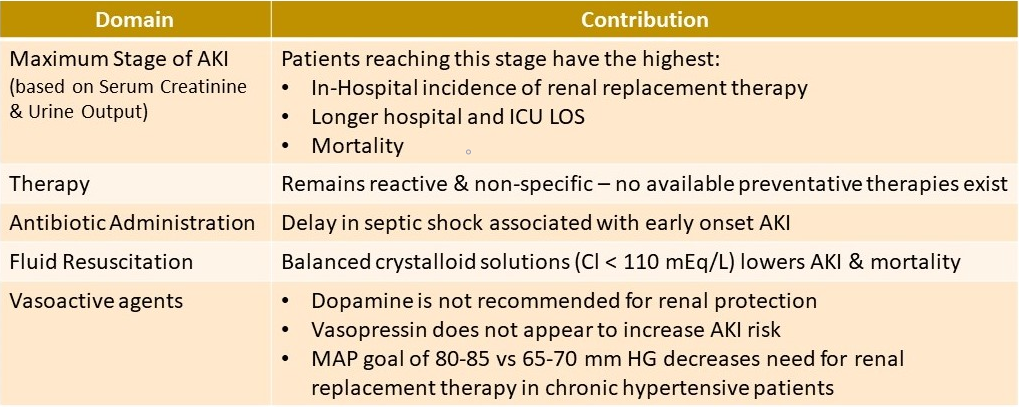
WHAT WE KNOW:
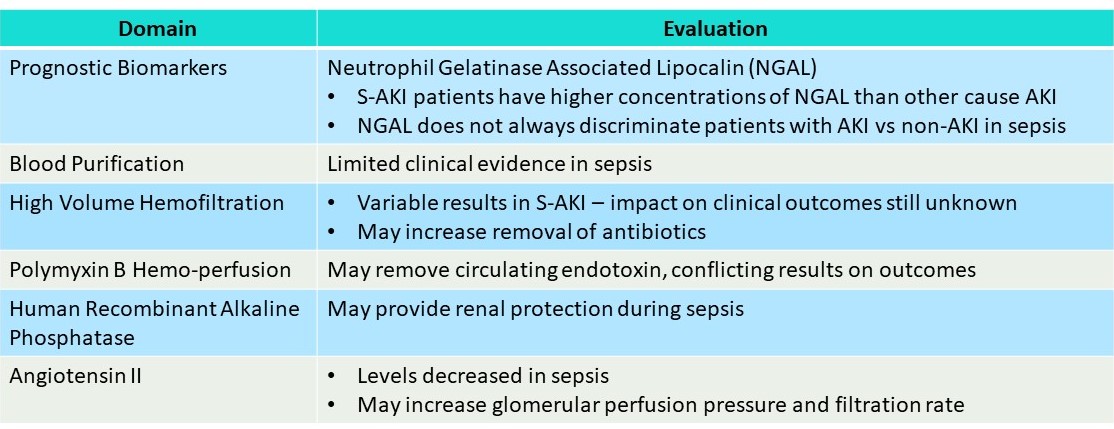
WHAT WE DO NOT KNOW (Ongoing Evaluations):
RECOVERY & LONG-TERM FOLLOW-UP:
- Numerous factors determine recovery and progression to chronic renal disease
- Close follow-up is important to promote renal recovery
- Special attention in S-AKI survivors for long term follow-up regarding chronic kidney disease include:
a. Recurrent sepsis and AKI episodes
b. Cardiovascular sequelae
CONCLUSIONS
- Patients with S-AKI have various clinical trajectories
- Early detection can help guide management but specific interventions are still lacking
- Long term follow up by a nephrologist after AKI requiring renal replacement therapy is associated with improved survival.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.