Is Time to Antibiotics a Good Metric for Sepsis?
SUMMARY
- Optimal antibiotic timing remains an actively debated topic.
- Sepsis is an extremely heterogeneous syndrome, therefore, with which characteristics do earlier antibiotic administration improve outcomes?
- A more nuanced process may be needed, rather than simply time to antibiotics.
BACKGROUND
- Sepsis is an extremely heterogeneous syndrome with a multitude of potential presentations.
- Recently attention has focused on the timeframe of antibiotic administration to improve sepsis-related mortality. Controversy exists regarding:
- The correct timeframe that antibiotic administration impacts outcomes.
- Differences between antibiotic order time vs administration time.
- Differences in treatment and outcomes within specific subgroups.
- Can specific factors determine which patients will benefit from early antibiotic administration?
REVIEW
- The most recent contribution to this topic was a retrospective review of 18,315 patients within a 7 hospital system from 2010 to 2016.
- 2 Major findings:
- Antibiotic administration in patients with sepsis is characterized as a
“J-Shaped Curve”
-
Antibiotics administered within the first hour had higher unadjusted mortality and prolonged length of stay (LOS).
-
LOS & mortality decreased over the next 3 hours
-
Then increased after 4 hours
-
- Antibiotic administration in patients with sepsis is characterized as a
Patients receiving antibiotics immediately upon arrival had higher mortality which was not achieved again until antibiotic administration equivalent to 8 hours after admission.
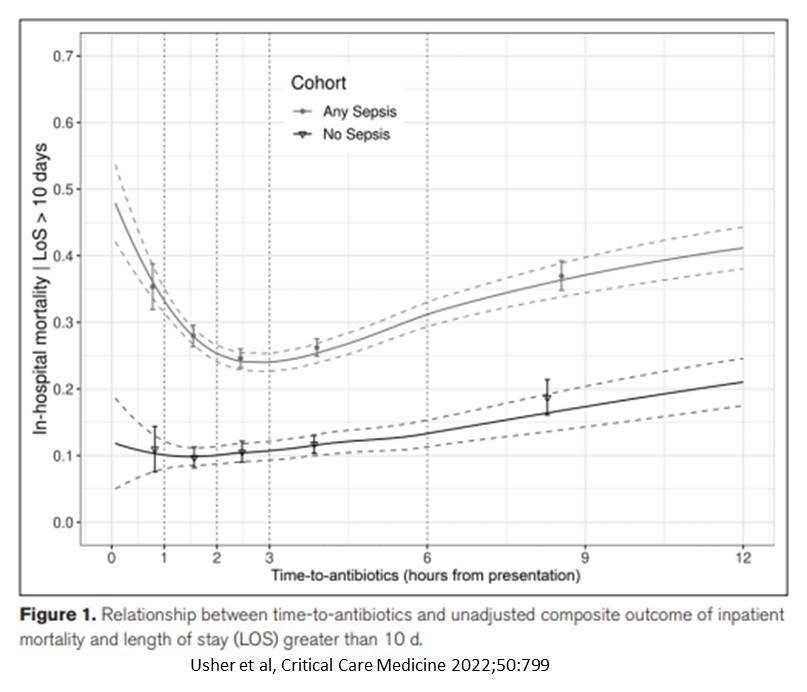
- When risk adjusted, earlier time to antibiotics was associated with better outcomes in all patients.
- Including patients with or without SIRS and organ dysfunction.
- Mortality and LOS decreased if antibiotics were administered prior to 2.5 hours after admission.
- LOS & mortality increased in all patients with antibiotics administered after 2.5 hours.
- Predictors of antibiotic timing fall into similar categories for patients with and without sepsis.
- In both groups of patients, lower antibiotic administration time is associated with improved outcomes if administered before 2.5 hours.
- Predictors of antibiotic-associated outcomes fell into similar categories for patients with and without sepsis.
- Temperature
- Respiratory Rate
- Diastolic Blood Pressure
- RBC distribution width
- Timeliness of antibiotic administration is not random, but influenced by patient characteristics.
CONCLUSIONS
- Patients receiving antibiotics earlier on admission were more likely to have higher illness acuity (shock, tachypnea, fever, elevated lactate).
- Patients receiving antibiotics later on admission were more likely to have a chronic illness (Liver dysfunction, Chronic Renal Disease, malignancy).
- Replacing Time-To-Antibiotic metric with a risk-adjustment to account for diverse patient presentations independent of sepsis may be a better metric.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





