Heart Rate & Temperature as Sepsis Mortality Prognostic Indicator
SUMMARY
-
The systemic effects of sepsis are due to the activation of a variety of physiologic cascades.
-
Activation of the sympathetic nervous system with catecholamine release and the acute inflammatory response results in elevations in temperature and heart rate.
-
The heart rate/Temperature ratio is a readily available indicator correlated with ICU mortality.
- Additional investigations are needed in order to establish the specific validation and thresholds for the heart rate/temperature ratio in sepsis patients.
REVIEW:
-
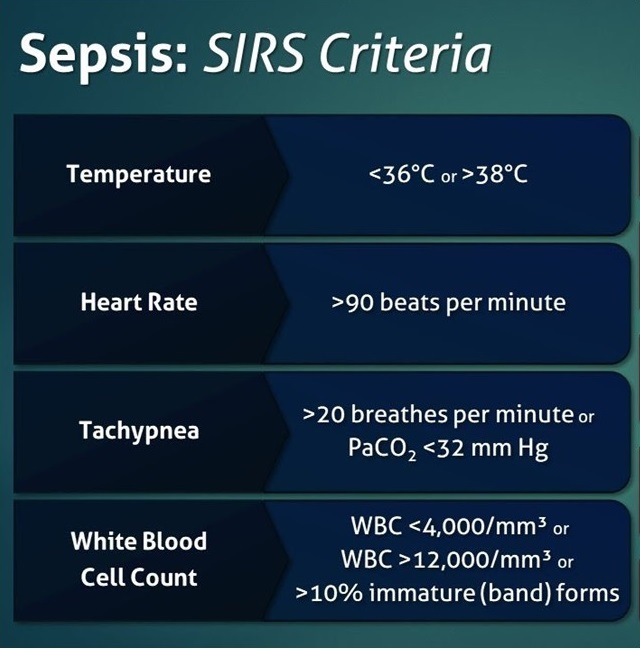
In 1992, the original Systemic Inflammatory Response Syndrome (SIRS) criteria was established.
-
- Inherent in these criteria are an elevated heart rate and hyper or hypothermia
-
The onset of sepsis initiates a number of complex pathophysiologic responses consisting of pro and anti-inflammatory responses, leading to:
- Cytokine release causing endothelial injury and possibly cell death
- Activation of coagulation factors impeding blood flow, leaky blood vessels and clot formation
- Interstitial fluid accumulation
- Excessive nitrous oxide production contributing to widespread hypotension and hemodynamic collapse
- These responses lead to tachycardia and hypo or hyperthermia
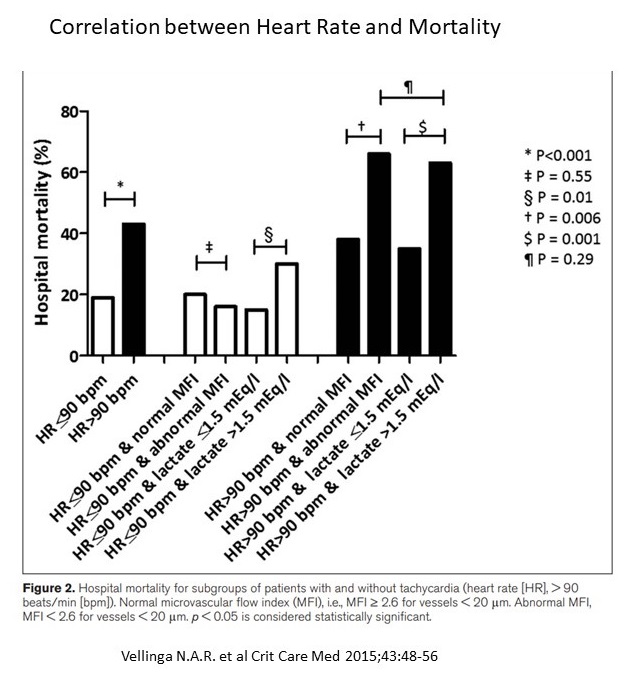
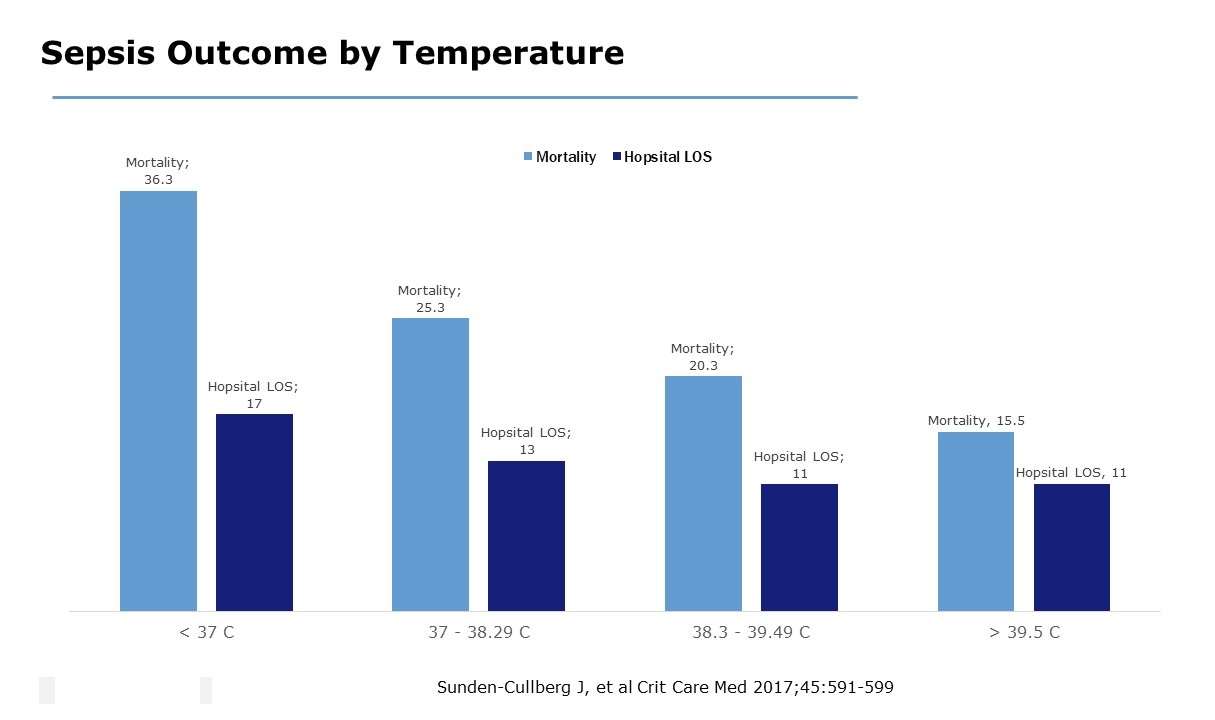
- There is a well established relationship between tachycardia or hypothermia with increased mortality.
Heart Rate & Temperature:
-
Commonly used, but impacted by a variety of other factors.
-
Heart Rate Index: Heart rate divided by temperature may provide a better indicator than either alone.
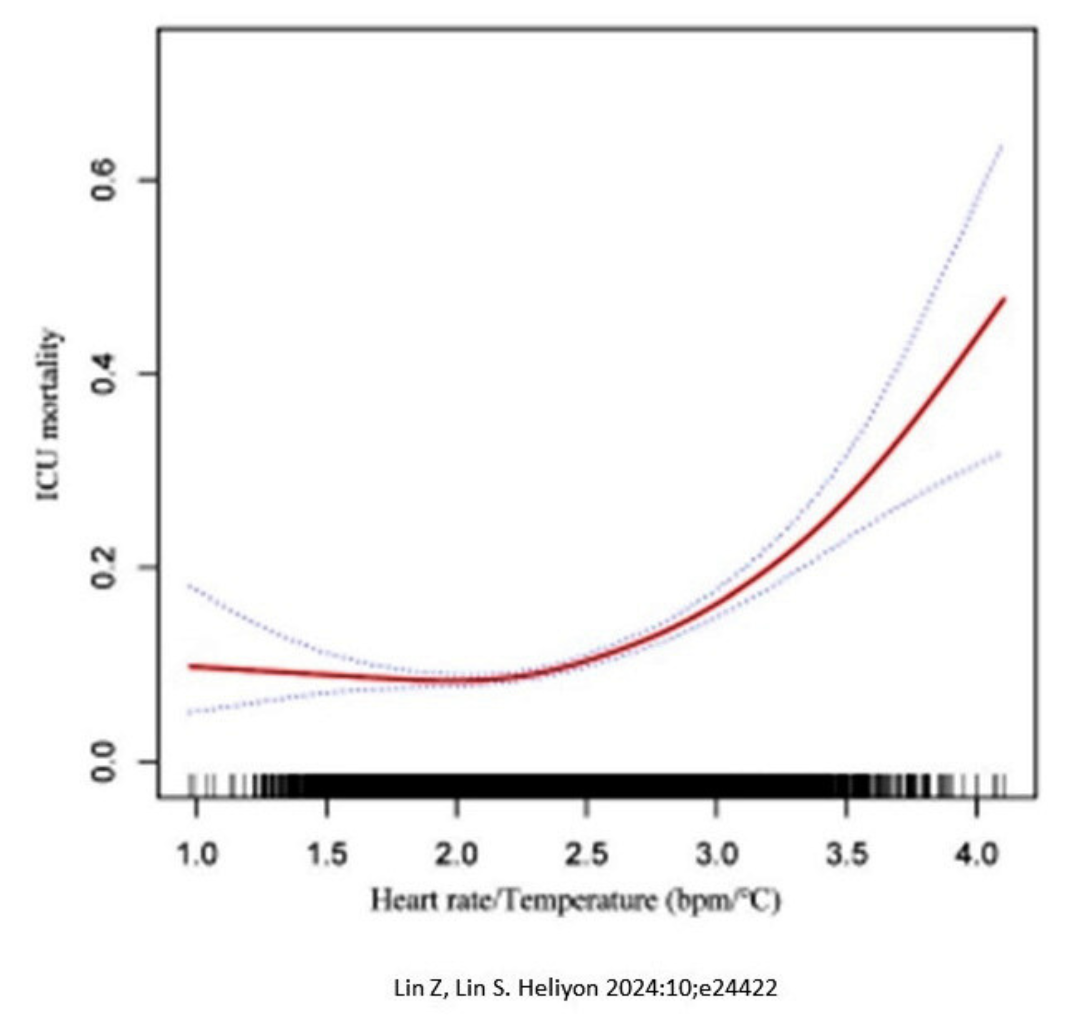
Lin Z & Lin S. Heartrate/temperature ratio: A practical prognostic indicator for critically ill patients with sepsis. Heliyon 2024;10:e24422.
-
12,321 patients with sepsis from MIMIC III database
-
1,309 non-survivors (10.62%)
- Non-survivors were (P<0.001):
- Older
- Higher heart rate
- Lower temperature
- Shorter hospital length of stay
-
The Heart Rate/Temperature ratio was found to be an independent risk factor for ICU death.
-
The inflection point was a ratio at 2.22
- Findings persisted when ratio was adjusted for: age, sex, SOFA mechanical ventilation, renal replacement therapy, heart failure, cardiac arrhythmias, valvular disease, peripheral vascular disease, pulmonary circulation disease, chronic pulmonary disease, hypothyroidism, hypertension, diabetes, renal failure, liver disease, tumor.
Additional Considerations:
-
The threshold value of 2.22 needs additional external validation as values may differ in various patient populations
-
Is one ratio sufficient to predict mortality, or are multiple (or continuous) ratios necessary
-
Should paired heart rate and temperature values be used to calculate the ratio, or should the worse value for each within a specified timeframe be used.
- What impact does the coadministration of concomitant pharmacologic agents have on the ratio (i.e. beta blockers, catecholamine administration, etc).
CONCLUSIONS
-
Heart rate and temperature are readily available parameters.
-
Elevated heart rate/temperature ratios are associated with increased ICU mortality rates in patients with sepsis.
-
Additional investigations are needed to validate the threshold and specific timing of vital sign attainment.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.