3 Key Factors When Using
Hospital Sepsis Discharge Data
Hospital Sepsis Discharge Data
SUMMARY
- Hospital discharge data is easy to obtain but may be misleading due to:
- Lack of clinical data
- Subject to documentation limitations
- Various identification strategies have been developed
- Conversion from ICD-9 to ICD-10 has expanded sepsis coding options resulting in different incidence rates and patterns.
REVIEW
Chan et al JACEP Open 2022;3:e12782
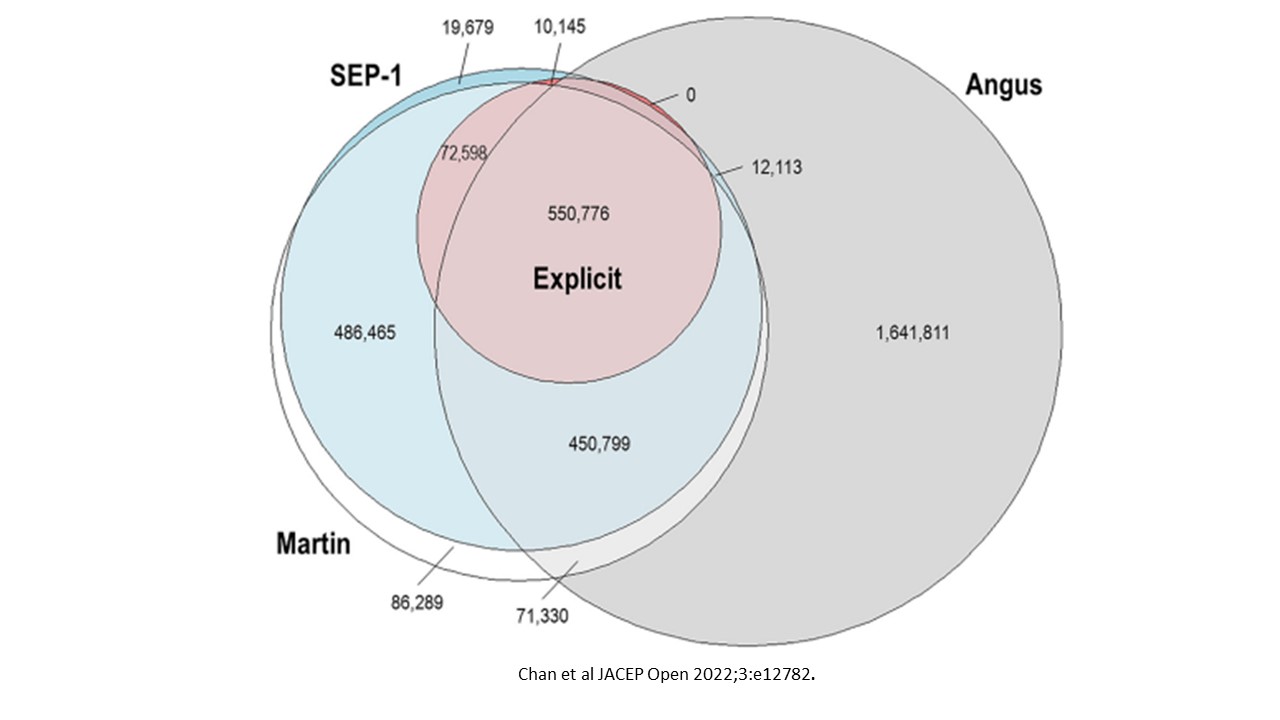
- January 1, 2016 – December 31, 2019 review of 3,424,339 discharged hospitalized sepsis cases
- Vizient database consisting of 50% of the nations acute care providers
- 97% of academic medical centers
- 20% of ambulatory providers.
- 4 sepsis identification strategies based on ICD-10 codes:
- Martin Method: all sepsis hospitalizations with at least 1 of 21 ICD-10 codes
- Angus Method: Any 1 of 892 ICD-10 codes for infection PLUS 1 of 47 ICD-10 codes for organ dysfunction
- CMS SEP-1 designation
- Explicit Method: ICD-10 codes R65.20 or R65.21
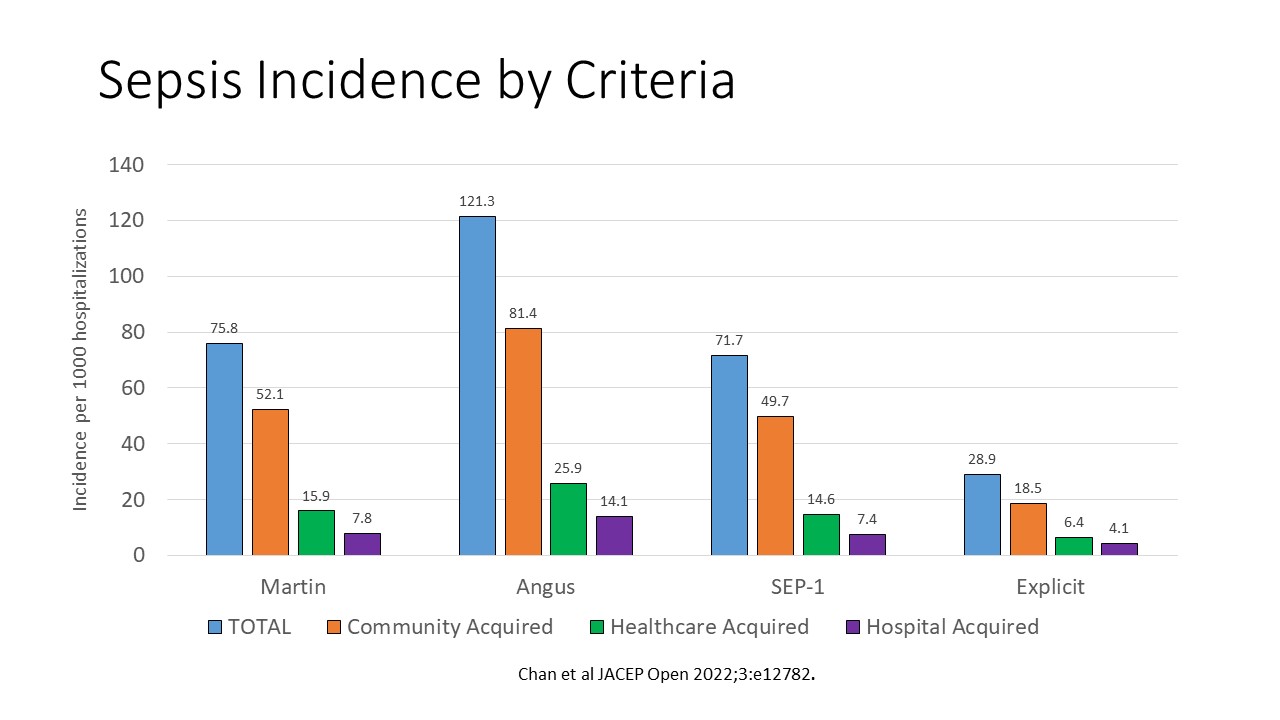
- Sepsis Subtypes:
- Community acquired sepsis (CAS)
- Healthcare associated sepsis (HCAS) – community acquired from inpatient nursing facilities, readmitted within 30 days or history of chronic hemodialysis.
- Hospital acquired sepsis (HAS) – not flagged as sepsis present on admission
KEY FACTOR #1: 4-fold variability in the incidence of sepsis based on criteria used
- Lowest incidence of sepsis was with the Explicit criteria (655,853 cases) vs highest incidence with the Angus criteria (1,845,027)
- A 4-fold increase
- Nearly half the cases were unique to the Angus criteria
- Similar cases associated with the remaining 3 criteria
KEY FACTOR #2: Sepsis present on admission remains the major type
- Incidence per 1000 hospitalizations shown in figure
- CAS (i.e. sepsis present on admission) remains the predominant finding
- HCAS is second most prevalent finding and a newly reported finding
- HAS (sepsis not documented on presentation) is the least prevalent.
- May be due to a missed diagnosis or sepsis development as a complication after admission
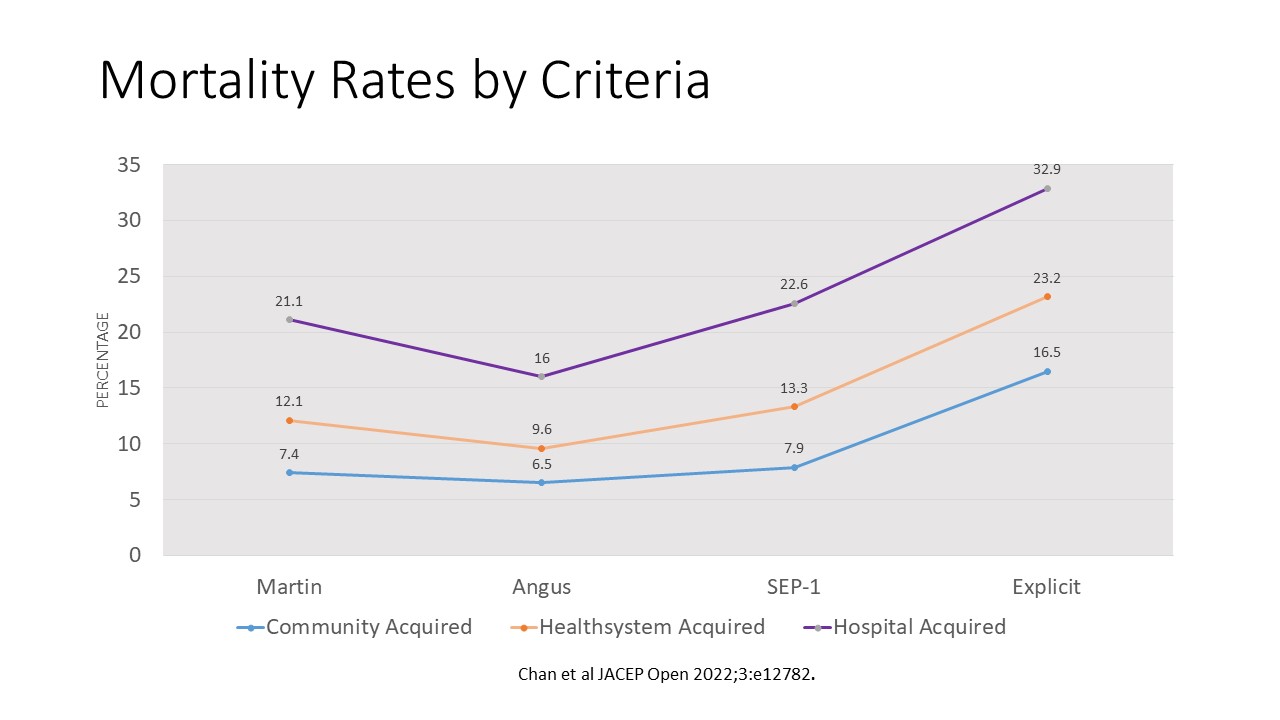
KEY FACTOR #3: HAS has the lowest incidence but poorest outcomes
- Regardless of the sepsis definition criteria used, HAS consistently has the lowest incidence
- However, it contributes the greatest negative outcomes
- Total length of stay (2.1 to 2.8 times higher than CAS)
- ICU length of stay (2 times higher than CAS)
- Hospital mortality (2.7 to 3.3 greater mortality risk compared to CAS)
CONCLUSIONS
- Using different criteria to define sepsis upon hospital discharge will dramatically affect incidence rates
- Sepsis present on admission remains the major source of sepsis patients
- Sepsis flagged as not present on admission is the lowest occurrence but has the poorest outcomes.
- Use of multiple criteria may offer a better strategy to identify and characterize sepsis based on discharge data.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





