Changes in Sepsis Trends: Real or Artificial?
SUMMARY
- Recent reports indicate a significant increase in the incidence of sepsis with a concomitant drop in mortality.
- Controversy exists over the true degree of change based on changing definitions and coding practices.
- Direct clinical indicators of infection and organ dysfunction are preferred over administrative codes.
BACKGROUND
- Sepsis remains a global issue with a recently reported 48.9 million cases worldwide.
- Sepsis remains one of the most expensive conditions in hospitals but accounts for less than 6% of all cases.
- Various reports tracking sepsis over the past decades have reported:
-
- Increasing actual numbers of sepsis cases annually
- Double digit rates of sepsis case increases
- Declining mortality rates at all severity levels of sepsis.
- Various explanations have been proposed for these changes and are listed below.
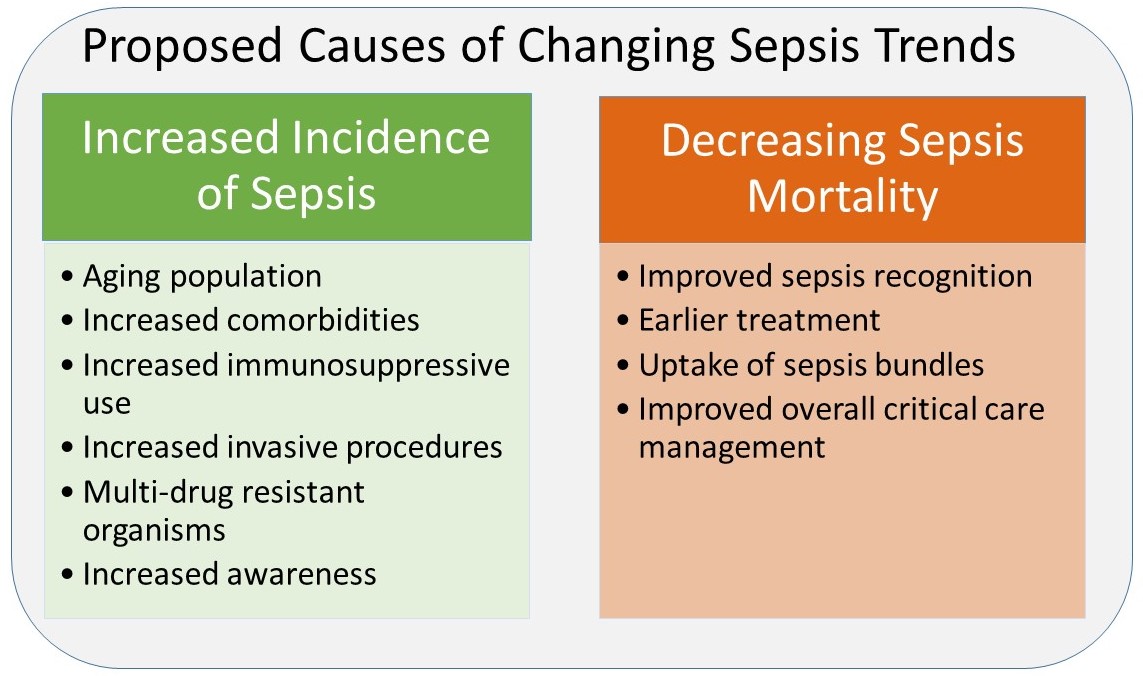
REVIEW
- Controversy exists over the degree of a true change in disease incidence and outcome versus artificial changes due to ever changing definitions and coding practices.
- Sepsis coding optimizes reimbursement
Coding Criteria Changes:
-
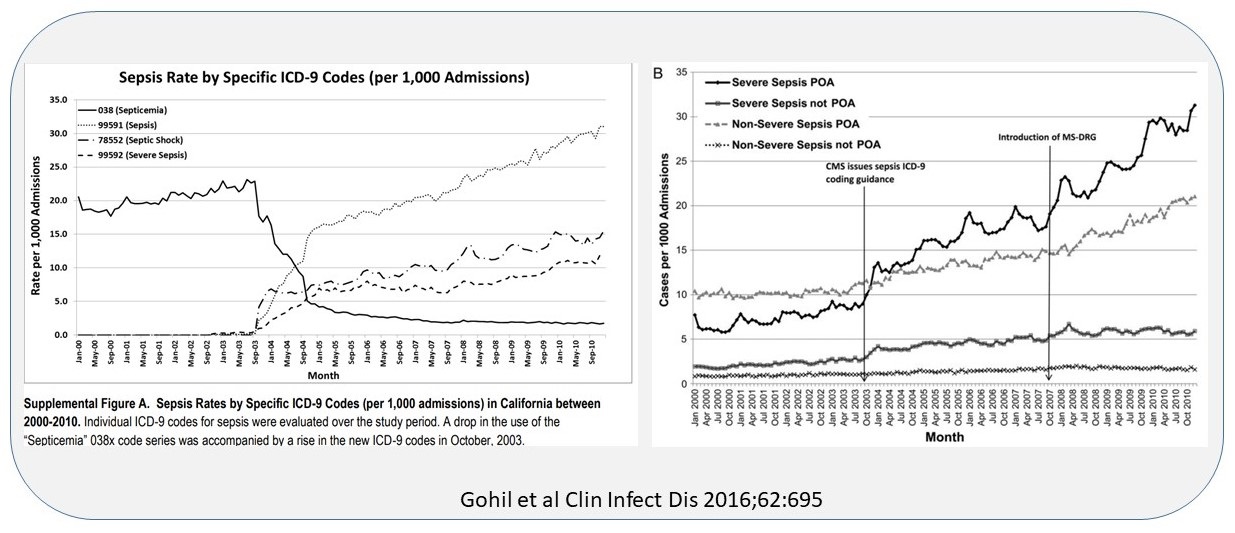
- October 2002: ICD-9 codes allowed for specific sepsis diagnosis within a single code.
- October 2003: CMS provides guidance on appropriate sepsis coding
- October 2007: CMD overhauls the previous Diagnosis Related Group reimbursement system to the “Medical Severity-Diagnosis Related Group” (MS-DRG) tying reimbursement to severity.
- A review of 635,780 severe sepsis cases from California from 2000-2010 saw annual hospitalization rates triple.
-
- Distinct sepsis hospitalization increases were seen following sepsis code changes.
- Overall California hospital admission rates had a non-significant change over the same time period.
- Comparing clinical criteria to discharge administrative codes in 57,273 patients with suspected infection and organ dysfunction from 2005 to 2013:
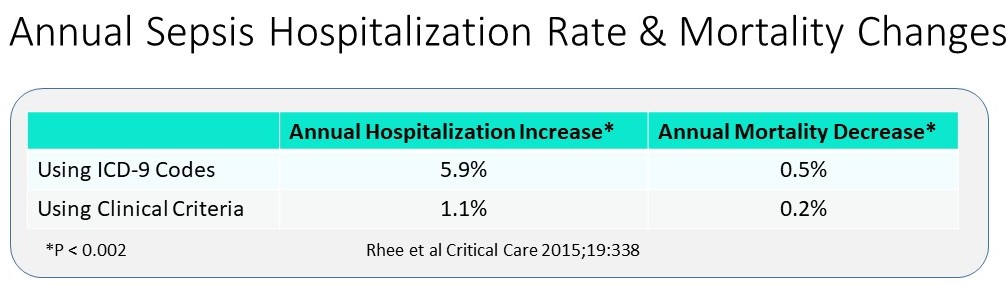
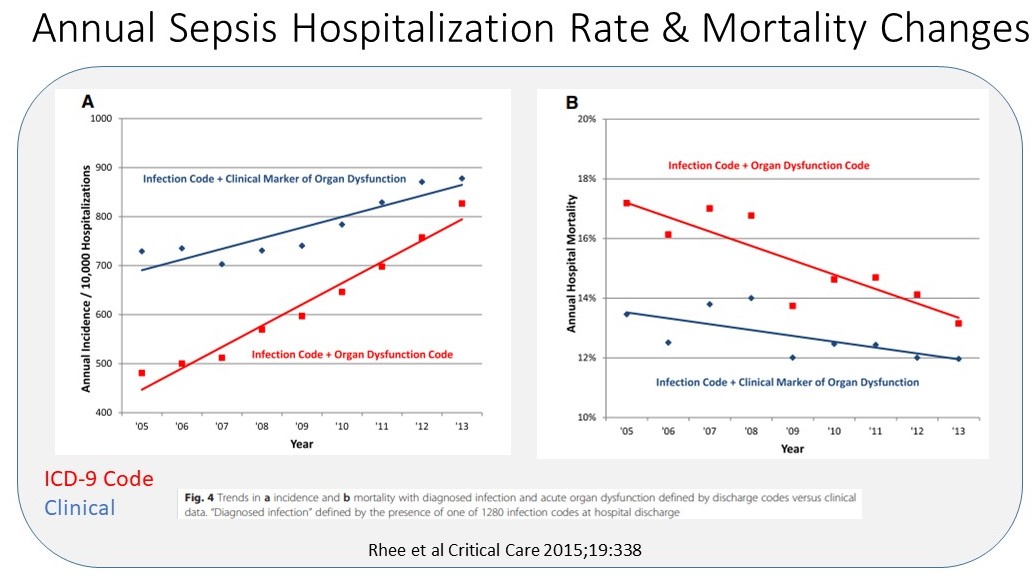
- If milder cases of disease are being documented and coded as sepsis, the increase number of cases and decreased mortality does not actually reflect improved outcomes.
CONCLUSIONS
- The lack of a “gold standard” diagnostic test coupled with highly subjective sepsis clinical criteria allows for discretion when coding for sepsis.
- Using objectively defined clinical criteria rather than administrative codes indicates that sepsis incidence and mortality rates have been essentially stable over the past decade.
- Measuring sepsis incidence, outcomes and trends should be based on data routinely found in the electronic health record.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





