3 Greatest Barriers and Approaches to Sepsis Program Implementations
SUMMARY
Implementation of an effective sepsis program is both time consuming and complicated. Each institution poses its own unique challenges. Despite this wide heterogeneity, 3 major common themes are the cause of much difficulty and confusion.
The key to success in sepsis program development is to develop a framework which address these common barriers. Sepsis identification and notification via clinical decision support systems; clinician buy-in and seamless integration into clinical workflow are important considerations. Each have unique potential solutions for program success.
BACKGROUND
Numerous approaches have been developed to identify and improve the outcome of sepsis. However, due to the considerable heterogeneity of sepsis, existing studies have not clearly demonstrated improved clinical outcomes. Some have questioned if a clinical decision support solution is even possible for sepsis given its nature as a continuum disease entity.
However, the implementation process is consistently far more difficult than anticipated. Barriers will impede, slow down or make implementation of a successful program very difficult.
Clinical acceptance is the most common barrier. There are at least 3 common barriers to clinician acceptance which will be identified and approaches provided below.
REVIEW
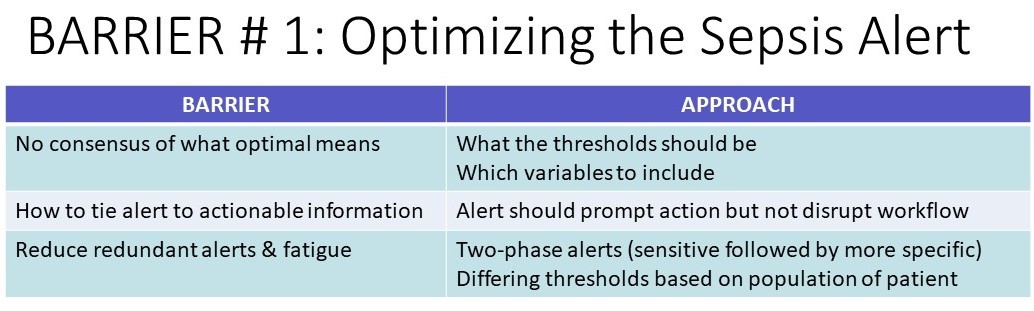
Barrier #1: The Sepsis Alert – Optimizing the alert
- No consensus of what optimal means
- How to tie alert to actionable information
- Reduce redundant alerts and alert fatigue
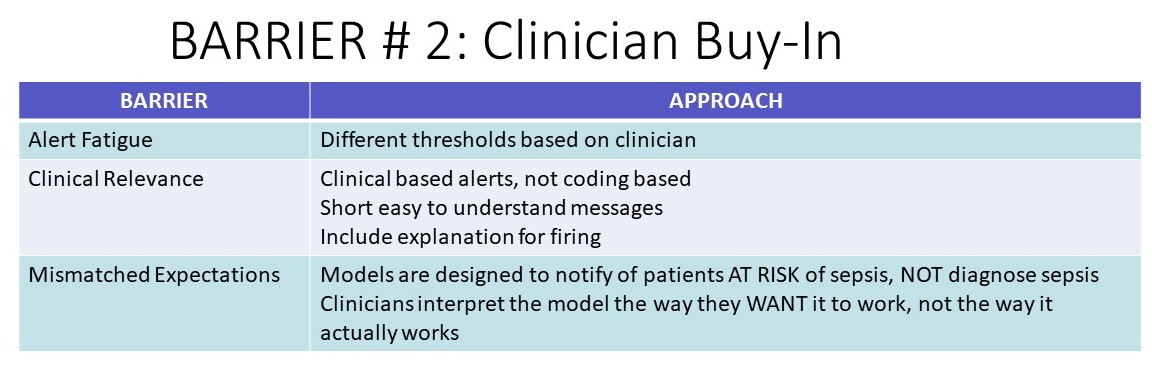
Barrier # 2: Clinician Buy In
- Alert fatigue
- Concerns about clinical relevance
- Mismatched expectations
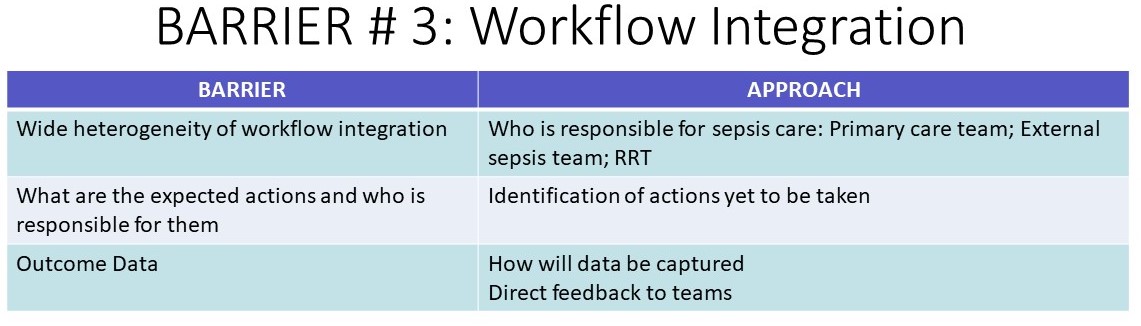
Barrier #3: Workflow Integration
- Wide heterogeneity of how programs are integrated into workflow
- What are the expected actions and who is responsible for these actions
- Outcome data
CONCLUSION
- Implementation of a sepsis program is time consuming and complicated
- Both rules based and machine learning notification systems pose significant challenges to optimize alerting and integration into workflow.
- Attention to initial and ongoing education, alert interpretation support and expectation management may improve the effectiveness of these programs.
To receive articles like these in your Inbox, you can subscribe to Sepsis Program Optimization Insights.
Erkan Hassan is the Co-Founder & Chief Clinical Officer of Sepsis Program Optimization where he designs & oversees the implementation of solutions to optimize sepsis programs.
To discuss your organization’s Barriers of Effective Sepsis Care, contact Erkan by phone (844) 4SEPSIS (844-473-7747), email (erkan@spo.icu), or video chat.





